A potential protection of melatonin on pathogenesis of oral sub-mucous fibrosis (OSMF) : a current update
Melatonin in oral submucous fibrosis
Abstract
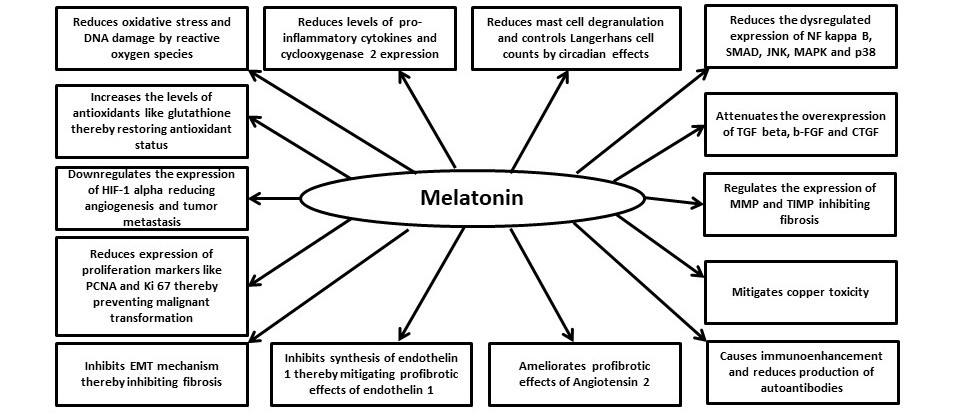
Oral submucous fibrosisis (OSMF) is a clinical condition of the oral cavity which is caused predominantly by areca nut consumption. This fibrotic condition affects almost all parts of the oral cavity and can cause significant reduction in mouth opening, thereby, resulting in functional impairment. The other potential risk of OSMF is its malignant transformation into oral squamous cell carcinoma, which occurs in a significant number of afflicted patients. Extensive researches have been conducted to understand the pathogenesis of OSMF for identification of tangible therapeutic modalities. To date, there is no effective therapeutic modality for this disorder. It is well known that melatonin has a potent anti-fibrotic, anti-oxidant, and pro-angiogenic effects. The therapeutic potential of melatonin on OSM cannot be ignored. In this article we have explored the potential mechanisms of melatonin as an adjuvant in the prevention and treatment of OSMF.
References
2. Gupta MK, Mhaske S (2008) Oral submucous fibrosis: Current concepts in etioathogenesis. People’s J. Sci. Res. 1: 39-44.
3. Schwartz (1952) Atrophia idiopathica mucosa oris. In: Demonstrated at the 11th International Dental Congress
4. Joshi S (1953) Fibrosis of the e palate and pillars. Ind. J. Otolaryngol. 4: 1-4.
5. Utsunomiya H, Tilakaratne WM, Oshiro K, Maruyama S, Suzuki M, Ida‐Yonemochi H, Cheng J, Saku T (2005) Extracellular matrix remodeling in oral submucous fibrosis: its stage‐specific modes revealed by immunohistochemistry and in situ hybridization. J. Oral. Pathol. Med. 34: 498-507. https://doi.org/10.1111/j.1600-0714.2005.00339.x.
6. Ranganathan K, Mishra G (2006) An overview of classification schemes for oral submucous fibrosis. J. Oral Maxillofac.Pathol. 10: 55–58.
7. Pindborg J (1966) Oral submucous fibrosis as a precancerous condition. J. Dent. Res. 45: 546–553.
8. Chen PH, Tsai CC, Lin YC, Ko YC, Yang YH, Shieh TY, Ho PS, Li CM, Min-Shan Ko A, Chen CH (2006) Ingredients contribute to variation in production of reactive oxygen species by areca quid. J. Toxicol. Environ. Heal. 69: 1055–1069. https://doi.org/10.1080/15287390500360224.
9. Arakeri G, Rai KK, Hunasgi S, Merkx MAW, Gao S, Brennan PA (2017) Oral submucous fibrosis: An update on current theories of pathogenesis. J. Oral Pathol. Med.46: 406–412. DOI: 10.1111/jop.12581.
10. Morgan MJ, Liu ZG (2011) Crosstalk of reactive oxygen species and NF-κB signaling. Cell Res. 21: 103–115.
11. Mithani SK, Mydlarz WK, Grumbine FL, Smith IM, Califano JA (2007) Molecular genetics of premalignant oral lesions. Oral Dis. 13: 126–133. DOI: 10.1111/j.1601-0825.2006.01349.x.
12. Tsai C-H, Chou M-Y, Chang Y-C (2003) The up-regulation of cyclooxygenase-2 expression in human buccal mucosal fibroblasts by arecoline: a possible role in the pathogenesis of oral submucous fibrosis. J. Oral Pathol. Med. 32: 146–153. https://doi.org/10.1034/j.1600-0714.2003.00004.x.
13. Jeng JH, Ho YS, Chan CP, Wang YJ, Hahn LJ, Lei D, Hsu CC, Chang MC (2000) Areca nut extract up-regulates prostaglandin production, cyclooxygenase-2 mRNA and protein expression of human oral keratinocytes. Carcinogenesis 21: 1365–1370. https://doi.org/10.1093/carcin/21.5.365.
14. Rai V, Bose S, Saha S, Chakraborty C (2019) Evaluation of oxidative stress and the microenvironment in oral submucous fibrosis. Heliyon 5: e01502. https://doi.org/10.1016/j.heliyon.2019.e01502.
15. Gupta S, Reddyand MVR, Harinath BC (2004) Role of oxidative stress and antioxidants in aetiopathogenesis and management of oral submucous fibrosis. Indian J. Clin. Biochem. 19: 138–141. https://doi.org/10.1007/BF02872409.
16. Lai K-C, Lee T-C (2006) Genetic damage in cultured human keratinocytes stressed by long-term exposure to areca nut extracts. Mutat. Res. Mol. Mech. Mutagen 599: 66–75. https://doi.org/10.1016/j.mrfmmm.2006.01.005.
17. Zhou ZS, Li M, Gao F, Peng JY, Xiao HB, Dai LX, Lin SR, Zhang R, Jin LY (2013) Arecoline suppresses HaCaT cell proliferation through cell cycle regulatory molecules. Oncol. Rep. 29: 2438–2444. https://doi.org/10.3892/or.2013.2360.
18. Narayanan B, Narasimhan M (2015) Langerhans cell expression in oral submucous fibrosis: an immunohistochemical analysis. J. Clin. Diagnostic Res. 9: ZC39.
19. Pujari R, Vidya N (2013) Mast cell density in oral submucous fibrosis : a possible role in pathogenesis. Int. J. Health Sci. (Qassim) 7: 23–29. https://doi.org/10.12816/0006017.
20. Kale AD, Mane DR, Shukla D (2013) Expression of transforming growth factor β and its correlation with lipodystrophy in oral submucous fibrosis: An immunohistochemical study. Med. Oral Patol. Oral Cir. Bucal 18: e12-e18. DOI: 10.4317/medoral.18226.
21. Pant I, Rao SG, Kondaiah P (2016) Role of areca nut induced JNK/ATF2/Jun axis in the activation of TGF-β pathway in precancerous Oral Submucous Fibrosis. Sci. Rep. 6: 1–15. https://doi.org/10.1038/srep34314.
22. Thomas GJ, Nystrom ML, Marshall JF (2006) αvβ6 integrin in wound healing and cancer of the oral cavity. J. Oral Pathol. Med. 35: 1–10. https://doi.org/10.1111/j.1600-0714.2005.00374.x.
23. Khan I, Kumar N, Pant I, Narra S, Kondaiah P. (2012) Activation of TGF-β pathway by areca nut constituents: a possible cause of oral submucous fibrosis. PLoS One 7: e51806. https://doi.org/10.1371/journal.pone.0051806.
24. Bishen KA, Radhakrishnan R, Satyamoorthy K (2008) The role of basic fibroblast growth factor in oral submucous fibrosis pathogenesis. J. Oral Pathol. Med. 37: 402–411. https://doi.org/10.1111/j.1600-0714.2008.00649.x.
25. Tsai CH, Yang SF, Chen YJ, Chou MY, Chang YC (2005) The upregulation of insulin-like growth factor-1 in oral submucous fibrosis. Oral Oncol. 41: 940–946. https://doi.org/10.1016/j.oraloncology.2005.05.006.
26. Deng YT, Chen HM, Cheng SJ, Chiang CP, Kuo MY (2009) Arecoline-stimulated connective tissue growth factor production in human buccal mucosal fibroblasts: Modulation by curcumin. Oral Oncol. 45: e99–e105. https://doi.org/10.1016/j.oraloncology.2009.04.004.
27. Illeperuma RP, Ryu MH, Kim KY, Tilakaratne WM, Kim J (2010) Relationship of fibrosis and the expression of TGF-β1, MMP-1, and TIMP-1 with epithelial dysplasia in oral submucous fibrosis. Oral Med. Pathol. 15: 21–28. https://doi.org/10.3353/omp.15.21.
28. Yang S-F, Tsai C-H, Chang Y-C (2008) The upregulation of heat shock protein 47 expression in human buccal fibroblasts stimulated with arecoline. J. Oral Pathol. Med. 37: 206–210. https://doi.org/10.1111/j.1600-0714.2007.00633.x.
29. Shetty SR, Babu SG, Kumari S, Rao V, Vijay R, Karikal A (2012) Malondialdehyde levels in oral sub mucous fibrosis: A clinicopathological and biochemical study. N. Am. J. Med. Sci. 4: 125–128. https://doi.org/10.4103/1947-2714.93887.
30. Ayinampudi BK, Narsimhan M (2012) Salivary copper and zinc levels in oral pre-malignant and malignant lesions. J. Oral Maxillofac. Pathol. 16: 178–182. https://doi.org/10.4103/0973-029X.98452.
31. Balakrishnan C, Aswath N (2015) Estimation of serum, salivary immunoglobulin G, immunoglobulin A levels and total protein, hemoglobin in smokeless tobacco chewers and oral submucous fibrosis patients. Contemp. Clin. Dent. 6: S157–S162. https://doi.org/10.4103/0976-237X.166820.
32. Santos CF, Morandini AC, Dionísio TJ, Faria FA, Lima MC, Figueiredo CM, Colombini-Ishikiriama BL, Sipert CR, Maciel RP, Akashi AP, Souza GP, Garlet GP, Rodini CO, Amaral SL, Becari C, Salgado MC, Oliveira EB, Matus I, Didier DN, Greene AS (2015) Functional local renin-angiotensin system in human and rat periodontal tissue. PLoS One 10: e0134601. https://doi.org/10.1371/journal.pone.0134601.
33. Ohuchi N, Koike K, Sano M, Kusama T, Kizawa Y, Hayashi K, Taniguchi Y, Ohsawa M, Iwamoto K, Murakami H (2002) Proliferative effects of angiotensin II and endothelin-1 on guinea pig gingival fibroblast cells in culture. Comp. Biochem. Physiol. C. Toxicol. Pharmacol. 132: 451–460. https://doi.org/10.1016/S1532-0456(02)00098-4.
34. Miyazaki M, Takai S, Jin D, Muramatsu M (2006) Pathological roles of angiotensin II produced by mast cell chymase and the effects of chymase inhibition in animal models. Pharmacol. Ther. 112: 668–676.
35. Shi-wen X, Kennedy L, Renzoni EA, Bou-Gharios G, du Bois RM, Black CM, Denton CP, Abraham DJ, Leask A (2007) Endothelin is a downstream mediator of profibrotic responses to transforming growth factor β in human lung fibroblasts. Arthritis Rheum. 56: 4189–4194. https://doi.org/10.1002/art.23134.
36. Ankita K, Shwetha V, Vanitha S, Reddy Sujatha S, Nagaraju R, Tupakula Pavan K (2019) Assessment of salivary endothelin-1 in patients with leukoplakia, submucous fibrosis, oral cancer and healthy individuals – a comparative study. J. Stomatol. Oral. Maxillofac. Surg. 120: 326–331. https://doi.org/10.1016/j.jormas.2019.02.024.
37. Yanjia H, Xinchun J (2007) The role of epithelial-mesenchymal transition in oral squamous cell carcinoma and oral submucous fibrosis. Clin. Chim. Acta. 383: 51–56.
38. Angadi P V, Kale AD, Hallikerimath S (2011) Evaluation of myofibroblasts in oral submucous fibrosis: Correlation with disease severity. J. Oral Pathol. Med. 40: 208–213. https://doi.org/10.1111/j.1600-0714.2010.00995.x.
39. Rao AR, Das P (1989) Evaluation of the carcinogenicity of different preparations of areca nut in mice. Int. J. Cancer 43: 728–732. https://doi.org/10.1002/ijc.2910430431.
40. Keshav R, Narayanappa U (2015) Expression of proliferating cell nuclear antigen (pcna) in oral submucous fibrosis: an immunohistochemical study. J. Clin. Diagnostic Res. 9: ZC20.
41. Iqbal A, Tamgadge S, Tamgadge A, Pereira T, Kumar S, Acharya S, Jadhav A (2020) Evaluation of Ki-67 expression in oral submucous fibrosis and its correlation with clinical and histopathological features. J. Microsc. Ultrastruct. 8: 20. https://doi.org/10.4103/jmau.jmau_28_19.
42. Pereira T, Surve R, Shetty S, Gotmare S (2020) Qualitative expression of hypoxia-inducible factor-1α in malignant transformation of oral submucous fibrosis: An immunohistochemical study. J. Oral Maxillofac. Pathol. 24: 106. https://doi.org/10.4103/jomfp.JOMFP_234_19.
43. Jirge V, Shashikanth M, Ali I, Anshumalee N (2008) Levamisole and antioxidants in the management of oral submucous fibrosis: a comparative study. J. Indian Acad. Oral Med. Radiol. 20: 135. https://doi.org/10.4103/0972-1363.52827.
44. Shetty P, Shenai P, Chatra L, Rao PK (2013) Efficacy of spirulina as an antioxidant adjuvant to corticosteroid injection in management of oral submucous fibrosis. Indian J. Dent. Res. 24: 347–350. https://doi.org/10.4103/0970-9290.118001.
45. Singh M, Niranjan HS, Mehrotra R, Sharma D, Gupta SC (2010) Efficacy of hydrocortisone acetate/hyaluronidase vs triamcinolone acetonide/hyaluronidase in the treatment of oral submucous fibrosis. Indian J. Med. Res.131: 665–669.
46. Alshadwi A, Bhatia I (2012) Excision of oral submucous fibrosis and reconstruction with full thickness skin graft: a case study and review of the literature. Case Rep. Dent. 2012: 628301.https://doi.org/10.1155/2012/628301.
47. Gupta A, Kukkar N, Sharif K, Main BJ, Albers CE, El-Amin III SF (2015) Bone graft substitutes for spine fusion: A brief review. World J. Orthop. 6: 449–456. https://doi.org/10.5312/wjo.v6.i6.449.
48. Arakeri G, Patil S, Maddur N, Rao US V, Subash A, Patil S, Gao S, Brennan PA (2020) Long‐term effectiveness of lycopene in the management of oral submucous fibrosis (OSMF): A 3‐years follow‐up study. J. Oral Pathol. Med. 49: 803–808. https://doi.org/10.1111/jop.13085.
49. Zechmeister L (1944) Cis-trans isomerization and stereochemistry of carotenoids and diphenyl-polyenes. Chem. Rev. 34: 267–344. https://doi.org/10.1021/cr60108a004.
50. Di Mascio P, Kaiser S, Sies H (1989) Lycopene as the most efficient biological carotenoid singlet oxygen quencher. Arch. Biochem. Biophys. 274: 532–538. https://doi.org/10.1016/0003-9861(89)90467-0.
51. Pennathur S, Maitra D, Byun J, Sliskovic I, Abdulhamid I, Saed GM, Diamond MP, Abu-Soud HM (2010) Potent antioxidative activity of lycopene: A potential role in scavenging hypochlorous acid. Free Radic. Biol. Med. 49: 205–213. https://doi.org/10.1016/j.freeradbiomed.2010.04.003.
52. Reiter RJ, Mayo JC, Tan DX, Sainz RM, Alatorre‐Jimenez M, Qin L (2016) Melatonin as an antioxidant: under promises but over delivers. J. Pineal Res. 61: 253–278.
53. Giannoulia-Karantana A, Vlachou A, Polychronopoulou S, Papassotiriou I, Chrousos GP (2007) Melatonin and immunomodulation: connections and potential clinical applications. Neuroimmunomodulation 13:133–144.
54. Reiter RJ (1991) Pineal melatonin: cell biology of its synthesis and of its physiological interactions. Endocr. Rev. 12:151–180. https://doi.org/10.1210/edrv-12-2-151.
55. Sugden D (1989) Melatonin biosynthesis in the mammalian pineal gland. Experientia 45: 922–932.
56. Tan DX, Manchester LC, Terron MP, Flores LJ, Reiter RJ (2007) One molecule, many derivatives: a never-ending interaction of melatonin with reactive oxygen and nitrogen species? J. Pineal Res. 42: 28–42.
57. Shimozuma M, Tokuyama R, Tatehara S, Umeki H, Ide S, Mishima K, Saito I, Satomura K (2011) Expression and cellular localizaion of melatonin-synthesizing enzymes in rat and human salivary glands. Histochem. Cell Biol. 135: 389–396. https://doi.org/10.1007/s00418-011-0800-8.
58. Madapusi BT, Rao SR (2018) Preliminary evaluation of human gingiva as an extrapineal site of melatonin biosynthesis in states of periodontal health and disease. J. Clin. Diagnostic Res.12: ZF01–ZF07. https://doi.org/10.7860/JCDR/2018/32451.11078.
59. Cagnacci A (1997) Influences of melatonin on human circadian rhythms. Chronobiol. Int. 14: 205–220.
60. Sharma S, Haldar C (2006) Melatonin prevents X-ray irradiation induced oxidative damagein peripheral blood and spleen of the seasonally breeding rodent, Funambulus pennanti during reproductively active phase. Int. J. Radiat. Biol. 82: 411–419. https://doi.org/10.1080/09553000600774105.
61. Tan D-X, Manchester LC, Reiter RJ, Plummer BF, Hardies LJ, Weintraub ST, Shepherd AM (1998) A novel melatonin metabolite, cyclic 3-hydroxymelatonin: abiomarker ofin vivohydroxyl radical generation. Biochem. Biophys. Res. Commun. 253: 614–620. https://doi.org/10.1006/bbrc.1998.9826.
62. Ressmeyer A-R, Mayo JC, Zelosko V, Sáinz RM, Tan DX, Poeggeler B, Antolín I, Zsizsik BK, Reiter RJ, Hardeland R (2003) Antioxidant properties of the melatonin metabolite N 1 -acetyl-5-methoxykynuramine (AMK): scavenging of free radicals and prevention of protein destruction. Redox. Rep. 8: 205–213. https://doi.org/10.1179/135100003225002709.
63. Xia M-Z, Liang Y-L, Wang H, Chen X, Huang YY, Zhang ZH, Chen YH, Zhang C, Zhao M, Xu DX, Song LH (2012) Melatonin modulates TLR4-mediated inflammatory genes through MyD88- and TRIF-dependent signaling pathways in lipopolysaccharide-stimulated RAW264.7 cells. J. Pineal Res. 53: 325–334. https://doi.org/10.1111/j.1600-079X.2012.01002.x.
64. Deng W-G, Tang S-T, Tseng H-P, Wu KK (2006) Melatonin suppresses macrophage cyclooxygenase-2 and inducible nitric oxide synthase expression by inhibiting p52 acetylation and binding. Blood 108: 518–524. https://doi.org/10.1182/blood-2005-09-3691.
65. Zhao X, Sun J, Su W, Shan H, Zhang B, Wang Y, Shabanova A, Shan H, Liang H (2018) Melatonin protects against lung fibrosis by regulating the hippo/YAP pathway. Int. J. Mol. Sci. 19: 1118. https://doi.org/10.3390/ijms19041118.
66. Lebda MA, Sadek KM, Abouzed TK, Tohamy HG, El-Sayed YS (2018) Melatonin mitigates thioacetamide-induced hepatic fibrosis via antioxidant activity and modulation of proinflammatory cytokines and fibrogenic genes. Life Sci. 192: 136–143. https://doi.org/10.1016/j.lfs.2017.11.036.
67. Wang H, Wei W, Wang NP, Gui SY, Wu L, Sun WY, Xu SY (2005) Melatonin ameliorates carbon tetrachloride-induced hepatic fibrogenesis in rats via inhibition of oxidative stress. Life Sci. 77: 1902–1915. https://doi.org/10.1016/j.lfs.2005.04.013.
68. Tahan V, Ozaras R, Canbakan B, Uzun H, Aydin S, Yildirim B, Aytekin H, Ozbay G, Mert A, Senturk H (2004) Melatonin reduces dimethylnitrosamine-induced liver fibrosis in rats. J. Pineal Res. 37: 78–84. https://doi.org/10.1111/j.1600-079X.2004.00137.x.
69. Czechowska G, Celinski K, Korolczuk A, Wojcicka G, Dudka J, Bojarska A, Reiter RJ (2015) Protective effects of melatonin against thioacetamide-induced liver fibrosis in rats. J. Physiol. Pharmacol. 66: 567–579.
70. Lee EJ, Lee MY, Chen HY, Hsu YS, Wu TS, Chen ST, Chang GL (2005) Melatonin attenuates gray and white matter damage in a mouse model of transient focal cerebral ischemia. J. Pineal Res. 38: 42–52. https://doi.org/10.1111/j.1600-079X.2004.00173.x.
71. Çikler E, Ercan F, Çetinel Ş, Contuk G, Şener G (2005) The protective effects of melatonin against water avoidance stress-induced mast cell degranulation in dermis. Acta Histochem. 106: 467–475. https://doi.org/10.1016/j.acthis.2004.10.001.
72. Prendergast BJ, Cable EJ, Patel PN, Pyter LM, Onishi KG, Stevenson TJ, Ruby NF, Bradley SP (2013) Impaired leukocyte trafficking and skin inflammatory responses in hamsters lacking a functional circadian system. Brain Behav. Immun. 32: 94–104. https://doi.org/10.1016/j.bbi.2013.02.007.
73. Wang Y rong, Hong R tao, Xie Y yuan, Xu J ming (2018) Melatonin ameliorates liver fibrosis induced by carbon tetrachloride in rats via inhibiting TGF-β1/Smad signaling pathway. Curr. Med. Sci. 38: 236–244. https://doi.org/10.1007/s11596-018-1871-8.
74. Osbek E, Ilbey YO, Ozbek M, Simsek A, Cekmen M, Somay A (2009) melatonin attenuates unilateral ureteral obstruction–induced renal injury by reducing. J. Endourol. 23: 1165–1173.
75. Choi HS, Kang JW, Lee SM (2015) Melatonin attenuates carbon tetrachloride-induced liver fibrosis via inhibition of necroptosis. Transl. Res. 166: 292–303. https://doi.org/10.1016/j.trsl.2015.04.002.
76. Turgut M, Öktem G, Uysal A, Yurtseven ME (2006) Immunohistochemical profile of transforming growth factor-β1 and basic fibroblast growth factor in sciatic nerve anastomosis following pinealectomy and exogenous melatonin administration in rats. J. Clin. Neurosci. 13: 753–758. https://doi.org/10.1016/j.jocn.2005.07.019.
77. Crespo I, San-Miguel B, Fernández A, De Urbina JO, González-Gallego J, Tuñón MJ (2015) Melatonin limits the expression of profibrogenic genes and ameliorates the progression of hepatic fibrosis in mice. Transl. Res. 165: 346–357. https://doi.org/10.1016/j.trsl.2014.10.003.
78. Hosseinzadeh A, Javad-Moosavi SA, Reiter RJ, Yarahmadi R, Ghaznavi H, Mehrzadi S (2018) Oxidative/nitrosative stress, autophagy and apoptosis as therapeutic targets of melatonin in idiopathic pulmonary fibrosis. Expert Opin. Ther. Targets 22:1049–1061.
79. Parmar P, Limson J, Nyokong T, Daya S (2002) Melatonin protects against copper-mediated free radical damage. J. Pineal Res. 32: 237–242. https://doi.org/10.1034/j.1600-079X.2002.01859.x.
80. Sharma R, Reiter RJ, Ma Q (2019) Melatonin: a hypothesis regarding its use to treat Wilson disease. Med. Hypotheses 133: 109408. https://doi.org/10.1016/j.mehy.2019.109408.
81. Lin GJ, Huang SH, Chen SJ, Wang CH, Chang DM, Sytwu HK (2013) Modulation by melatonin of the pathogenesis of inflammatory autoimmune diseases. Int. J. Mol. Sci. 14:11742–11766.
82. Ohashi N, Ishigaki S, Isobe S (2019) The pivotal role of melatonin in ameliorating chronic kidney disease by suppression of the renin–angiotensin system in the kidney. Hypertens. Res. 42:761–768.
83. León J, Casado J, Jiménez Ruiz SM, Zurita MS, González‐Puga C, Rejón JD, Gila A, Muñoz de Rueda P, Pavón EJ, Reiter RJ, Ruiz‐Extremera A (2014) Melatonin reduces endothelin-1 expression and secretion in colon cancer cells through the inactivation of FoxO-1 and NF-κβ. J. Pineal Res. 56: 415–426. https://doi.org/10.1111/jpi.12131.
84. Yu N, Sun YT, Su XM, He M, Dai B, Kang J (2016) Melatonin attenuates TGFβ1-induced epithelial-mesenchymal transition in lung alveolar epithelial cells. Mol. Med. Rep. 14: 5567–5572. https://doi.org/10.3892/mmr.2016.5950.
85. Jung-Hynes B, Schmit TL, Reagan-Shaw SR, Siddiqui IA, Mukhtar H, Ahmad N (2011) Melatonin, a novel Sirt1 inhibitor, imparts antiproliferative effects against prostate cancer in vitro in culture and in vivo in TRAMP model. J. Pineal Res. 50: 140–149. https://doi.org/10.1111/j.1600-079X.2010.00823.x.
86. Park SY, Jang WJ, Yi EY, Jang JY, Jung Y, Jeong JW, Kim YJ (2010) Melatonin suppresses tumor angiogenesis by inhibiting HIF-1α stabilization under hypoxia. J. Pineal Res. 48: 178–184. https://doi.org/10.1111/j.1600-079X.2009.00742.x.

This work is licensed under a Creative Commons Attribution 4.0 International License.
For all articles published in Melatonin Res., copyright is retained by the authors. Articles are licensed under an open access Creative Commons CC BY 4.0 license, meaning that anyone may download and read the paper for free. In addition, the article may be reused and quoted provided that the original published version is cited. These conditions allow for maximum use and exposure of the work, while ensuring that the authors receive proper credit.
In exceptional circumstances articles may be licensed differently. If you have specific condition (such as one linked to funding) that does not allow this license, please mention this to the editorial office of the journal at submission. Exceptions will be granted at the discretion of the publisher.


