Melatonergic index as a prognostic biomarker of reproductive organ cancers: correlations with metabolic parameters as well as clock genes PER1 and TIMELESS
Melatonergic system on reproductive organ cancers
Abstract
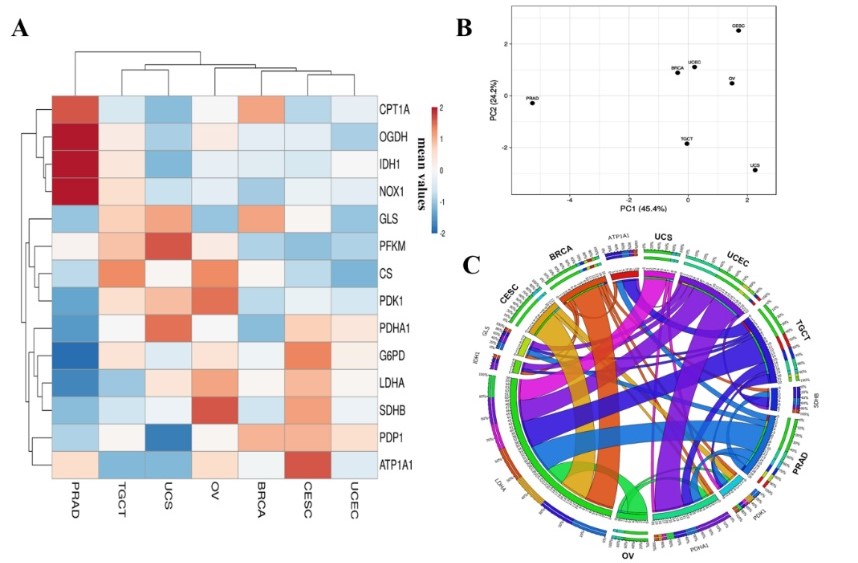
Cancers of the reproductive organs are often hard to be detected, and patients’ survival rate drops considerably even when the tumor is removed. Based on the fact that melatonin levels are significantly lower in cancer cells than that in the healthy cells, and this melatonin suppression remains during tumor progression, we have examined a simple two-gene-based melatonergic system [the indices of melatonin synthesis and metabolism (ASMT:CYP1A1, ASMT:CYP1A2, ASMT:CYP1B1)] as a prognostic factor for reproductive organ cancer survival rate. RNA-seq data from The Cancer Genome Atlas (TCGA) of seven types of human reproductive organ tumors (n = 3571 samples) were analyzed. By stratifying the set of index values into high vs low risk, we observed that patients with a high melatonergic index had improved survival rates for cervical, ovarian, and endometrial cancers. Patients at high-risk (low melatonergic index) showed a trend of diagnosis of breast, prostate, and testicular cancers at the younger age, while patients with cervical, ovarian, and endometrial cancers presented with higher tumor staging. The melatonergic indices, especially the ASMT:CYP1B1, positively correlated with the clock gene PER1 while negatively correlated with the clock gene TIMELESS in all reproductive organ cancers. We further analyzed the correlation between the expression profiles of the melatonin-synthesizing enzyme (ASMT gene) with metabolic enzyme-encoding genes. Notably, LDHA, PDK1, and PDHA1 showed a higher correlation in male and female reproductive organ tumors, while IDH1, SDHB, GLS, and ATP1A1 had a positive correlation in breast, testicular, and endometrial cancers. These results have provided a comprehensive evaluation of the melatonergic system in relation to the reproductive organ tumor microenvironment and identified promising gene signatures as potential biomarkers for cancer diagnostics, prognostics, and therapeutics.
References
2. Weiderpass E, Labrèche F (2012) Malignant tumors of the female reproductive system. Saf. Health Work 3 (3):166-180. DOI: 10.5491/SHAW.2012.3.3.166.
3. Rajitha B, Malla RR, Vadde R, et al. (2021) Horizons of nanotechnology applications in female specific cancers. Semin. Cancer Biol. 69: 376-390. DOI: 10.1016/j.semcancer.2019.07.005.
4. Chuffa LG, Lupi-Junior LA, Costa AB, et al. (2017) The role of sex hormones and steroid receptors on female reproductive cancers. Steroids 118: 93-108. DOI: 10.1016/j.steroids.2016.12.011.
5. Gann PH (2002) Risk factors for prostate cancer. Rev. Urol. 4: S3-S10.
6. McGlynn KA & Trabert B (2012) Adolescent and adult risk factors for testicular cancer. Nat. Rev. Urol. 9 (6):.339-349. DOI: 10.1038/nrurol.2012.61.
7. Aggarwal S, Verma SS, Aggarwal S, Gupta SC (2021) Drug repurposing for breast cancer therapy: Old weapon for new battle. Semin. Cancer Biol. 68: 8-20. DOI: 10.1016/j.semcancer.2019.09.012.
8. Hardeland R, Madrid JA, Tan D-X, et al. (2011) Melatonin, the circadian multioscillator system and health: the need for detailed analyses of peripheral melatonin signaling. J. Pineal Res. 52 (2): 139-166. DOI: 10.1111/j.1600-079x.2011.00934.x.
9. Reiter RJ, Sharma R, Ma Q, et al. (2020) Circadian and non-circadian melatonin: influences on glucose metabolism in cancer cells. J. Curr. Sci. Technol. 10 (1): 95-98. DOI: 10.14456/jcst.2020.9.
10. de Almeida Chuffa LG, Seiva FRF, Cucielo MS, et al. (2018) Mitochondrial functions and melatonin: a tour of the reproductive cancers. Cell Mol. Life Sci. 76 (5): 837-863. DOI: 10.1007/s00018-018-2963-0.
11. Chuffa LGdA, Reiter RJ, & Lupi LA (2017) Melatonin as a promising agent to treat ovarian cancer: molecular mechanisms. Carcinogenesis 38 (10): 945-952. DOI: 10.1093/carcin/bgx054.
12. Chuffa LGdA, Carvalho RF, Justulin LA, et al. (2020) A meta‐analysis of microRNA networks regulated by melatonin in cancer: Portrait of potential candidates for breast cancer treatment. J. Pineal Res. 69 (4): DOI: 10.1111/jpi.12693.
13. Chuffa LGA, Fioruci-Fontanelli BA, Mendes LO, et al. (2015) Melatonin attenuates the TLR4-mediated inflammatory response through MyD88- and TRIF-dependent signaling pathways in an in vivo model of ovarian cancer. BMC cancer 15: 34-34. DOI: 10.1186/s12885-015-1032-4.
14. Shafabakhsh R, Reiter RJ, Mirzaei H, et al. (2019) Melatonin: A new inhibitor agent for cervical cancer treatment. J. Cell Physiol. 234 (12): 21670-21682. DOI: 10.1002/jcp.28865.
15. Pariente R, Pariente JA, Rodríguez AB, et al. (2015) Melatonin sensitizes human cervical cancer HeLa cells to cisplatin-induced cytotoxicity and apoptosis: effects on oxidative stress and DNA fragmentation. J. Pineal Res. 60 (1): 55-64. DOI: 10.1111/jpi.12288.
16. Hevia D, Mayo JC, Quiros I, et al. (2010) Monitoring intracellular melatonin levels in human prostate normal and cancer cells by HPLC. Anal. Bioanal. Chem. 397 (3): 1235-1244. DOI: 10.1007/s00216-010-3653-4.
17. Tan D-X, Hardeland R, Back K, et al. (2016) On the significance of an alternate pathway of melatonin synthesis via 5-methoxytryptamine: comparisons across species. J. Pineal Res. 61 (1): 27-40. DOI: 10.1111/jpi.12336.
18. Ma X, Idle JR, Krausz KW, et al. (2004) Metabolism of melatonin by human cytochromes P450. Drug Metab. Dispos. 33 (4): 489-494. DOI: 10.1124/dmd.104.002410.
19. Kinker GS, Oba-Shinjo SM, Carvalho-Sousa CE, et al. (2015) Melatonergic system-based two-gene index is prognostic in human gliomas. J. Pineal Res. 60 (1): 84-94. DOI: 10.1111/jpi.1229.
20. Lv J-W, Zheng Z-Q, Wang Z-X, et al. (2019) Pan-cancer genomic analyses reveal prognostic and immunogenic features of the tumor melatonergic microenvironment across 14 solid cancer types. J. Pineal Res. 66 (3): e12557. DOI: 10.1111/jpi.12557.
21. Angelousi A, Kassi E, Ansari-Nasiri N, et al. (2019) Clock genes and cancer development in particular in endocrine tissues. Endocr. Relat. Cancer 26 (6): R305-R317. DOI: 10.1530/erc-19-0094.
22. Mohd Azmi NAS, Juliana N, Mohd Fahmi Teng NI, et al. (2020) Consequences of circadian disruption in shift workers on chrononutrition and their psychosocial well-being. Int. J. Environ. Res. Public. Health 17 (6): 2043. DOI: 10.3390/ijerph17062043.
23. Morales-Santana S, Morell S, Leon J, et al. (2019) An Overview of the Polymorphisms of Circadian Genes Associated With Endocrine Cancer. Front. Endocrinol. (Lausanne) 10: 104-104. DOI: 10.3389/fendo.2019.00104.
24. Angelousi A, Kassi E, Nasiri-Ansari N, et al. (2018) Clock genes alterations and endocrine disorders. Eur. J. Clin. Invest. 48 (6): e12927. DOI: 10.1111/eci.12927.
25. Chuffa LGdA, Seiva FRF, Cucielo MS, et al. (2019) Clock genes and the role of melatonin in cancer cells: an overview. Melatonin Res. 2 (2): 133-157. DOI: 10.32794/mr11250026.
26. Kobayashi Y, Banno K, Kunitomi H, et al. (2018) Warburg effect in Gynecologic cancers. J. Obstet. Gynaecol. Res. 45 (3): 542-548. DOI: 10.1111/jog.13867.
27. Zhong Y, Li X, Ji Y, et al. (2017) Pyruvate dehydrogenase expression is negatively associated with cell stemness and worse clinical outcome in prostate cancers. Oncotarget 8 (8): 13344-13356. DOI: 10.18632/oncotarget.14527.
28. Reiter RJ, Sharma R, Ma Q, Rosales-Corral S, de Almeida Chuffa LG (2020) Melatonin inhibits Warburg-dependent cancer by redirecting glucose oxidation to the mitochondria: a mechanistic hypothesis. Cell Mol. Life Sci. 77: 2527-2542. DOI: 10.1007/s00018-019-03438-1.
29. Blask DE, Dauchy RT, Dauchy EM, et al. (2014) Light exposure at night disrupts host/cancer circadian regulatory dynamics: impact on the Warburg effect, lipid signaling and tumor growth prevention. PLoS One 9: e102776. DOI: 10.1371/journal.pone.0102776.
30. Reiter RJ, Sharma R, Ma Q (2021) Switching diseased cells from cytosolic aerobic glycolysis to mitochondrial oxidative phosphorylation: A metabolic rhythm regulated by melatonin? J. Pineal Res. 70: e12677. DOI: 10.1111/jpi.12677.
31. Tomczak K, Czerwińska P, Wiznerowicz M (2015) The Cancer Genome Atlas (TCGA): an immeasurable source of knowledge. Contemp. Oncol. (Pozn) 19 (1A): A68-A77. DOI: 10.5114/wo.2014.47136.
32. Tang Z, Li C, Kang B, et al. (2017) GEPIA: a web server for cancer and normal gene expression profiling and interactive analyses. Nucleic Acids Res. 45 (W1): W98-W102. DOI: 10.1093/nar/gkx247.
33. Goldman MJ, Craft B, Hastie M, et al. (2020) Visualizing and interpreting cancer genomics data via the Xena platform. Nat. Biotechnol. 38 (6): 675-678. DOI: 10.1038/s41587-020-0546-8.
34. Metsalu T & Vilo J (2015) Clust Vis: a web tool for visualizing clustering of multivariate data using Principal Component Analysis and heatmap. Nucleic Acids Res. 43 (W1):W566-W570. DOI: 10.1093/nar/gkv468.
35. Fernandes PA, Kinker GS, Navarro BV, et al. (2021) Melatonin-Index as a biomarker for predicting the distribution of presymptomatic and asymptomatic SARS-CoV-2 carriers. Melatonin Res. 4 (1): 189-205. DOI: 10.32794/mr11250090.
36. Grin W & Grünberger W (1998) A Significant Correlation between Melatonin Deficiency and Endometrial Cancer. Gynecol. Obstet. Invest. 45 (1): 62-65. DOI: 10.1159/000009926.
37. Zhao M, Wan J, Zeng K, et al. (2016) The reduction in circulating melatonin level may contribute to the pathogenesis of ovarian cancer: a retrospective study. J. Cancer 7 (7): 831-836. DOI: 10.7150/jca.14573.
38. Karasek M, Kowalski AJ, Suzin J, et al. (2005) Serum melatonin circadian profiles in women suffering from cervical cancer. J. Pineal Res. 39 (1): 73-76. DOI: 10.1111/j.1600-079x.2005.00221.x.
39. González-González A, Mediavilla MD, Sánchez-Barceló, EJ (2018) Melatonin: a molecule for reducing breast cancer risk. Molecules 23 (2): 336. DOI: 10.3390/molecules23020336.
40. Zare H, Shafabakhsh R, Reiter RJ, Asemi Z (2019) Melatonin is a potential inhibitor of ovarian cancer: molecular aspects. J. Ovarian Res. 12 (1): 26. DOI: 10.1186/s13048-019-0502-8.
41. Zhao Q, Wang W, Cui J (2019) Melatonin enhances TNF-α-mediated cervical cancer HeLa cells death via suppressing CaMKII/Parkin/mitophagy axis. Cancer Cell Int. 19: 58. DOI: 10.1186/s12935-019-0777-2.
42. Gu C, Yang H, Chang K, et al. (2020) Melatonin alleviates progression of uterine endometrial cancer by suppressing estrogen/ubiquitin C/SDHB-mediated succinate accumulation. Cancer Lett. 476: 34-47. DOI: 10.1016/j.canlet.2020.02.009.
43. Mayo J, Hevia D, Quiros-Gonzalez I, et al. (2017) IGFBP3 and MAPK/ERK signaling mediates melatonin-induced antitumor activity in prostate cancer. J. Pineal Res. 62 (1): e12373. DOI: 10.1111/jpi.12373.
44. Li H-X (2019) The role of circadian clock genes in tumors. Onco. Targets Ther. 12: 3645-3660. DOI: 10.2147/OTT.S203144.
45. Miller BH, McDearmon EL, Panda S, et al. (2007) Circadian and CLOCK-controlled regulation of the mouse transcriptome and cell proliferation. Proc. Natl. Acad. Sci. U S A 104 (9): 3342-3347. DOI: 10.1073/pnas.0611724104.
46. Truong T, Liquet B, Menegaux F, et al. (2014) Breast cancer risk, nightwork, and circadian clock gene polymorphisms. Endocr. Relat. Cancer 21 (4): 629-638. DOI: 10.1530/erc-14-0121.
47. Fu A, Leaderer D, Zheng T, et al. (2011) Genetic and epigenetic associations of circadian gene TIMELESS and breast cancer risk. Mol. Carcinog 51 (12): 923-929. DOI: 10.1002/mc.20862.
48. Reszka E, Przybek M, Muurlink O, et al. (2017) Circadian gene variants and breast cancer. Cancer Lett. 390: 137-145. DOI: 10.1016/j.canlet.2017.01.012.
49. van der Watt PJ, Roden LC, Davis KT, et al. (2020) Circadian oscillations persist in cervical and esophageal cancer cells displaying decreased expression of tumor-suppressing circadian clock genes. Mol. Cancer Res. 18 (9): 1340-1353. DOI: 10.1158/1541-7786.mcr-19-1074.
50. Zhang W, He W, Shi Y, et al. (2016) Aberrant TIMELESS expression is associated with poor clinical survival and lymph node metastasis in early-stage cervical carcinoma. Int. J. Oncol. 50 (1): 173-184. DOI: 10.3892/ijo.2016.3784.
51. Wang Z, Wang H, Wang Z, et al. (2020) Associated analysis of PER1/TUBB2B with endometrial cancer development caused by circadian rhythm disorders. Med. Oncol. 37 (10): DOI: 10.1007/s12032-020-01415-4.
52. Sartorelli LS, Bombardi Neto RJ, Mosqueta-Pinheiro MG, et al. (2021) Blood melatonin level can serve as a potential biomarker for prostate and hepatocellular carcinomas. Melatonin Res. 4 (2): 253-269: DOI: 10.32794/mr11250094.
53. Reiter RJ, Sharma R, Zuccari DAPC, et al. (2021) Melatonin synthesis in and uptake by mitochondria: implications for diseased cells with dysfunctional mitochondria. Future Med. Chem. 13 (4): 335-339. DOI: 10.4155/fmc-2020-0326.
54. Reiter RJ, Sharma R, & Rosales-Corral S (2021) Anti-Warburg effect of melatonin: a proposed mechanism to explain its inhibition of multiple diseases. Int. J. Mol. Sci. 22 (2): 764. DOI: 10.3390/ijms22020764.
55. Reiter RJ, Sharma R, Ma Q, et al. (2019) Inhibition of mitochondrial pyruvate dehydrogenase kinase: a proposed mechanism by which melatonin causes cancer cells to overcome cytosolic glycolysis, reduce tumor biomass and reverse insensitivity to chemotherapy. Melatonin Res. 2 (3): 105-119. DOI: 10.32794/mr11250033.

This work is licensed under a Creative Commons Attribution 4.0 International License.
For all articles published in Melatonin Res., copyright is retained by the authors. Articles are licensed under an open access Creative Commons CC BY 4.0 license, meaning that anyone may download and read the paper for free. In addition, the article may be reused and quoted provided that the original published version is cited. These conditions allow for maximum use and exposure of the work, while ensuring that the authors receive proper credit.
In exceptional circumstances articles may be licensed differently. If you have specific condition (such as one linked to funding) that does not allow this license, please mention this to the editorial office of the journal at submission. Exceptions will be granted at the discretion of the publisher.


