Melatonin stimulates extracellular matrix formation in human articular cartilage chondrocytes
Melatonin stimulates human chondrocytes.
Abstract
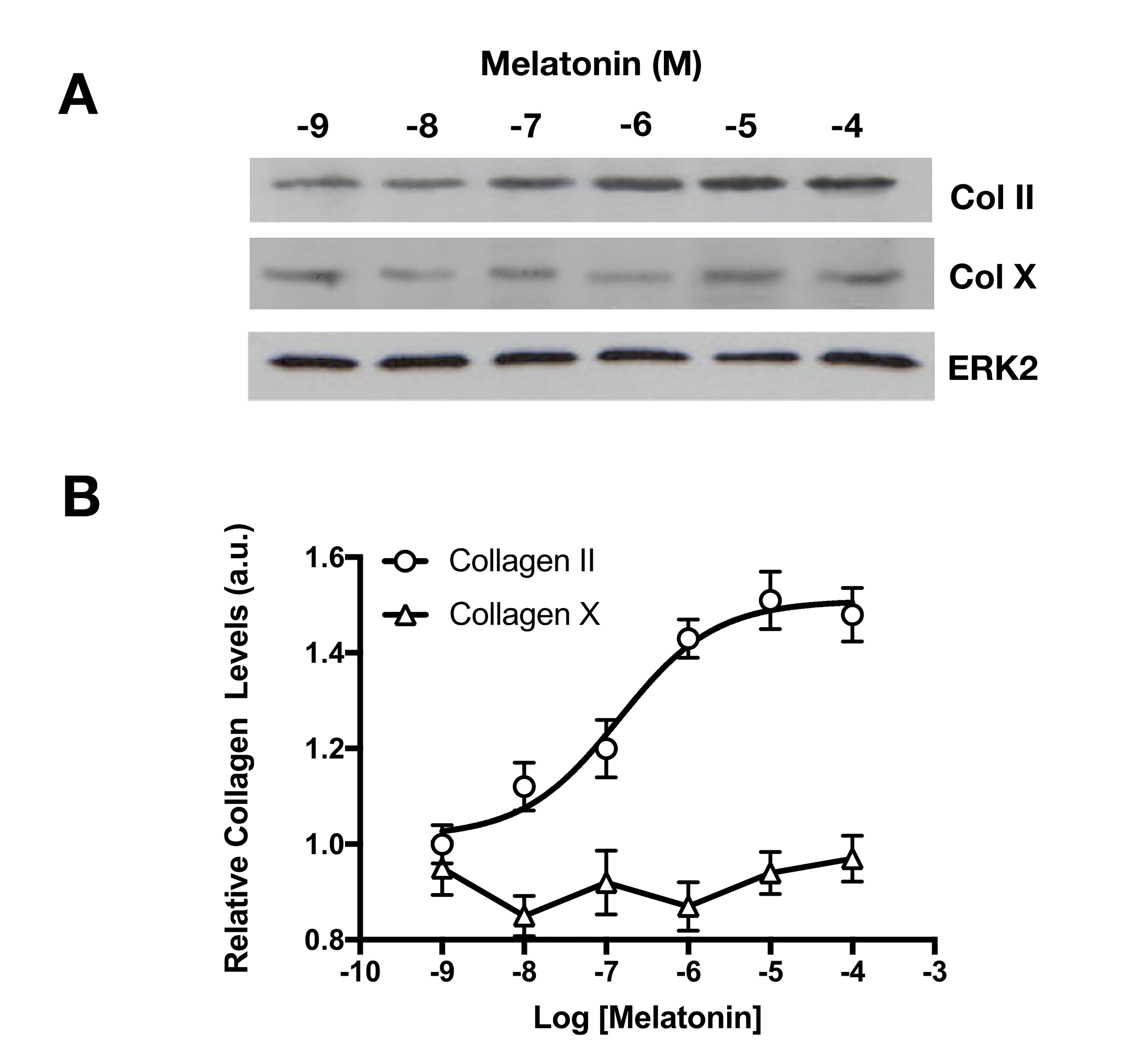
The articular cartilage present in joints is permanently subjected to physical stress, thus producing injuries and consequently pain. Chondrocytes are responsible for repairing this damage, but often the reparation tissue is inadequate. The application of melatonin to human articular chondrocytes may be a better solution, by generating a good extracellular matrix. Human chondrocytes were assayed in the presence of melatonin, demonstrating that these cells generate more extracellular matrix indicated by the increased Alcian blue staining. This effect of melatonin was concentration- dependent and presented a pD2 value of 6.8 ± 0.1 (n=5). Melatonin also significantly promotes the production of collagen II quantified by western-blot analysis. The effect of melatonin on the collagen II production is also concentration-dependence, with a pD2 value of 6.9 ± 0.2 (n=5). In contrast, melatonin had little effect on the collagen X. The antagonistic study by its non-selective membrane receptor blocker luzindole or its MT2 specific blocker DH-97 identified that these actions of melatonin are mediated by melatonin membrane receptors, mainly by MT2. In summary, melatonin stimulates the production of extracellular matrix and collagen II in chondrocytes and these actions may have significantly clinical implications since it may benefit the autologous chondrocyte transplantations, the only way to maintain and repair the damaged cartilage.
References
2. Tsumaki N (2018) Cartilage/chondrocyte research and osteoarthritis. Regeneration of articular cartilage damage using iPS cell-derived cartilage. Clin. Calcium 28 (6): 803-808.
3. Lopez-Alcorocho JM, et al. (2018) Cartilage defect treatment using high-density autologous chondrocyte implantation: two-year follow-up. Cartilage 9 (4): 363-369.
4. Chang CC, et al. (2018) Protective effect of melatonin against oxidative stress-induced apoptosis and enhanced autophagy in human retinal pigment epithelium cells. Oxid. Med. Cell Long. 2018: 9015765.
5. Manchester LC, et al. (2015) Melatonin: an ancient molecule that makes oxygen metabolically tolerable. J. Pineal Res. 59 (4): 403-419.
6. Calvo JR, Gonzalez-Yanes C, & Maldonado MD (2013) The role of melatonin in the cells of the innate immunity: a review. J. Pineal Res. 55 (2): 103-120.
7. Alarma-Estrany P & Pintor J (2007) Melatonin receptors in the eye: location, second messengers and role in ocular physiology. Pharmacol. Therapeutics 113 (3): 507-522.
8. Jockers R, et al. (2016) Update on melatonin receptors: IUPHAR Review 20. Br. J. Pharmacol. 173 (18): 2702-2725.
9. Hosseinzadeh A, et al. (2016) Apoptosis signaling pathways in osteoarthritis and possible protective role of melatonin. J. Pineal Res. 61 (4): 411-425.
10. Zhang Z, et al. (2019) Melatonin protects vertebral endplate chondrocytes against apoptosis and calcification via the Sirt1-autophagy pathway. J. Cell Mol. Med. 23 (1): 177-193.
11. Huang CC, et al. (2019) Melatonin attenuates TNF-alpha and IL-1beta expression in synovial fibroblasts and diminishes cartilage degradation: implications for the treatment of rheumatoid arthritis. J. Pineal Res. e12560: doi: 10.1111/jpi.12560.
12. Maestroni GJ, Sulli A, Pizzorni C, Villaggio B, & Cutolo M (2002) Melatonin in rheumatoid arthritis: synovial macrophages show melatonin receptors. Ann. NY. Acad. Sci. USA 966: 271-275.
13. Lunstrum GP, et al. (1999) Chondrocyte differentiation in a rat mesenchymal cell line. J. Histochem. Cytochem. 47 (1): 1-6.
14. Pei M, He F, Wei L, & Rawson A (2009) Melatonin enhances cartilage matrix synthesis by porcine articular chondrocytes. J. Pineal Res. 46 (2): 181-187.
15. Tiku ML & Madhan B (2016) Preserving the longevity of long-lived type II collagen and its implication for cartilage therapeutics. Ageing Res. Rev. 28: 62-71.
16. Shen G (2005) The role of type X collagen in facilitating and regulating endochondral ossification of articular cartilage. Orthodon. Craniofacial Res. 8 (1): 11-17.
17. Hollander AP, et al. (1995) Damage to type II collagen in aging and osteoarthritis starts at the articular surface, originates around chondrocytes, and extends into the cartilage with progressive degeneration. J. Clin. Invest. 96 (6): 2859-2869.
18. McDonough AL (1981) Effects of immobilization and exercise on articular cartilage-a review of literature. J. Orto. Sport Phys. Ther. 3 (1): 2-5.
19. Armstrong SJ, Read RA, Ghosh P, & Wilson DM (1993) Moderate exercise exacerbates the osteoarthritic lesions produced in cartilage by meniscectomy: a morphological study. Osteoarthr. Cartil. 1 (2): 89-96.
20. Armiento AR, Alini M, & Stoddart MJ (2018) Articular fibrocartilage - Why does hyaline cartilage fail to repair? Adv. Drug Deliver Rev. doi 10/1016/j.addr.218.12.015.
21. Amis AA (2001) Evaluating the healing of articular cartilage defects. J. Bone Joint Surg. 83A (10):1591-1592.
22. Bae DK, Yoon KH, & Song SJ (2006) Cartilage healing after microfracture in osteoarthritic knees. Arthroscopy 22 (4): 367-374.
23. Buckwalter JA (1998) Articular cartilage: injuries and potential for healing. J. Ortho. Sport Phys. Ther. 28 (4): 192-202.
24. Campbell CJ (1969) The healing of cartilage defects. Clin. Ortho. Rel. Res. 64: 45-63.

This work is licensed under a Creative Commons Attribution 4.0 International License.
For all articles published in Melatonin Res., copyright is retained by the authors. Articles are licensed under an open access Creative Commons CC BY 4.0 license, meaning that anyone may download and read the paper for free. In addition, the article may be reused and quoted provided that the original published version is cited. These conditions allow for maximum use and exposure of the work, while ensuring that the authors receive proper credit.
In exceptional circumstances articles may be licensed differently. If you have specific condition (such as one linked to funding) that does not allow this license, please mention this to the editorial office of the journal at submission. Exceptions will be granted at the discretion of the publisher.


