Effects of melatonin on the circadian functions of sleep-wake cycle, metabolism, hormonal regulation and immune activity: A recent review
Circadian rhythms and melatonin: Recent review
Abstract
Rhythms following a period of approximately 24 hours are called circadian (from Latin circa diem, approximately one day) rhythms. These rhythms are observed in the activities of various vital body functions. Melatonin is considered as an important molecule participating in the formation of circadian rhythms of virtually all organisms. As a molecular regulator of the circadian clock, melatonin has various regulatory functions in both physiological and pathological conditions. Sleep-wake cycle depends on CSF melatonin levels, and melatonin also has a protective effect on the disrupted sleep-wake cycle in various pathological conditions. Melatonin ensures the proper function of vital metabolic pathways; therefore, it improves metabolism-related systems and protects them from damage. A bidirectional relationship between hormonal activity and melatonin ensures it having a healing effect on various reproductive disorders. Finally, melatonin can target inflammation pathways and various elements of immune system by changing their behavior and structure. In summary, melatonin has important effects on vital body functions mediated by its receptors, signaling pathways and clock genes, and has the capacity to protect and improve these functions under pathological conditions.
References
2. Patke A, Young MW, Axelrod S (2019) Molecular mechanisms and physiological importance of circadian rhythms. Nat. Rev. Mol. Cell Biol. 21: 67-84.
3. Se J, et al. (2019) Genome-wide association analyses of chronotype in 697, 828 individuals provides insights into circadian rhythms. Yearb. Paediatr. Endocrinol. 10.1530/ey.16.1.1.
4. Fu L, Lee CC (2003) The circadian clock: pacemaker and tumour suppressor. Nat. Rev. Cancer 3: 350-361.
5. Hardeland R, et al. (2011) Melatonin—A pleiotropic, orchestrating regulator molecule. Prog. Neurobiol. 93: 350-384.
6. Macchi MM, Bruce JN (2004) Human pineal physiology and functional significance of melatonin. Front. Neuroendocrinol. 25: 177-195.
7. Moore RY, Klein DC (1974) Visual pathways and the central neural control of a circadian rhythm in pineal serotonin N-acetyltransferase activity. Brain Res. 71: 17-33.
8. Lewy AJ, Ahmed S, Jackson JM L, Sack RL (1992) Melatonin shifts human orcadian rhythms according to a phase-response curve. Chronobiol. Int. 9: 380-392.
9. Tordjman S, et al. (2017) Melatonin: Pharmacology, functions and therapeutic benefits. Curr. Neuropharmacol. 15: 434-443.
10. Zisapel N (2018) New perspectives on the role of melatonin in human sleep, circadian rhythms and their regulation. Br. J. Pharmacol. 175: 3190-3199.
11. Fowler S, Hoedt EC, Talley NJ, Keely S, Burns GL (2022) Circadian rhythms and melatonin metabolism in patients with disorders of gut-brain interactions. Front. Neurosci. 16: 825246-825246.
12. Takahashi JS, (2017) Transcriptional architecture of the mammalian circadian clock. Nat. Rev. Genet. 18: 164-179.
13. Cao X, Yang Y, Selby CP, Liu Z, Sancar A (2021) Molecular mechanism of the repressive phase of the mammalian circadian clock. Proc. Natl. Acad. Sci. USA. 118: e2021174118.
14. Cho H, et al. (2012) Regulation of circadian behaviour and metabolism by REV-ERB-α and REV-ERB-β. Nature 485: 123-127.
15. Lee JM, Kim H, Baek SH (2021) Unraveling the physiological roles of retinoic acid receptor-related orphan receptor α. Exp. Mol. Med. 53: 1278-1286.
16. Yoshitane H, et al. (2019) Functional D-box sequences reset the circadian clock and drive mRNA rhythms. Commun. Biol. 2: 300-300.
17. Ono D, Yamanaka A (2017) Hypothalamic regulation of the sleep/wake cycle. Neurosci. Res. 118: 74-81.
18. Waterhouse J, Fukuda Y, Morita T (2012) Daily rhythms of the sleep-wake cycle. J. Physiol. Anthropol. 31: 5-5.
19. Okechukwu CE (2022) The neurophysiologic basis of the human sleep–wake cycle and the physiopathology of the circadian clock: a narrative review. Egypt. J. Neurol. Psychiatry Neurosurg. 58: 34.
20. Poisson A, et al. (2019) Smith-magenis syndrome: Molecular basis of a genetic-driven melatonin circadian secretion disorder. Int. J. Mo.l Sci. 20: 3533.
21. Brown RE, Basheer R, McKenna JT, Strecker RE, McCarley RW (2012) Control of sleep and wakefulness. Physiol. Rev. 92: 1087-1187.
22. Moon E, Partonen T, Beaulieu S, Linnaranta O (2022) Melatonergic agents influence the sleep-wake and circadian rhythms in healthy and psychiatric participants: a systematic review and meta-analysis of randomized controlled trials. Neuropsychopharmacology 47: 1523-1536.
23. Xia T, et al. (2016) Melatonin pretreatment prevents isoflurane-induced cognitive dysfunction by modulating sleep–wake rhythm in mice. Brain Res.1634: 12-20.
24. Yin X-L, et al. (2022) Melatonin pretreatment prevents propofol-induced sleep disturbance by modulating circadian rhythm in rats. Exp. Neurol. 354: 114086.
25. Koch BCP, et al. (2009) Effects of nocturnal hemodialysis on melatonin rhythm and sleep-wake behavior: An uncontrolled trial. Am. J. Kidney Dis. 53: 658-664.
26. Koch BCP, Nagtegaal JE, Hagen EC, Wee PMT, Kerkhof GA (2010) Different melatonin rhythms and sleep–wake rhythms in patients on peritoneal dialysis, daytime hemodialysis and nocturnal hemodialysis. Sleep Med. 11: 242-246.
27. Ba-Ali S, et al.(2019) Assessment of diurnal melatonin, cortisol, activity, and sleep−wake cycle in patients with and without diabetic retinopathy. Sleep Med. 54: 35-42.
28. Li W, et al. (2019) Disruption of sleep, sleep-wake activity rhythm, and nocturnal melatonin production in breast cancer patients undergoing adjuvant chemotherapy: prospective cohort study. Sleep Med. 55: 14-21.
29. Tanner N, et al. (2022) Effectiveness of melatonin treatment for sleep disturbance in orthopaedic trauma patients: A prospective, randomized control trial. Injury 53: 3945-3949.
30. Santoro SD, Giacheti CM, Rossi NF, Campos LMG, Pinato L (2016) Correlations between behavior, memory, sleep-wake and melatonin in Williams-Beuren syndrome. Physiol. Behav. 159: 14-19.
31. De Leersnyder H (2006) Inverted rhythm of melatonin secretion in Smith–Magenis syndrome: from symptoms to treatment. Trends Endocrinol. Metab. 17: 291-298.
32. Williams SR, Zies D, Mullegama SV, Grotewiel MS, Elsea SH (2012) Smith-Magenis syndrome results in disruption of CLOCK gene transcription and reveals an integral role for RAI1 in the maintenance of circadian rhythmicity. Am. J. Hum. Genet. 90: 941-949.
33. Potocki L, et al. (2000) Circadian rhythm abnormalities of melatonin in Smith-Magenis syndrome. J. Med. Genet. 37: 428-433.
34. Polymeropoulos CM, et al. (2021) Tasimelteon safely and effectively improves sleep in Smith-Magenis syndrome: a double-blind randomized trial followed by an open-label extension. Genet. Med. 23: 2426-2432.
35. Cullell N, et al. (2021) Sleep/wake cycle alterations as a cause of neurodegenerative diseases: A Mendelian randomization study. Neurobiol. Aging 106: 320.e321-320.e312.
36. Bolitho SJ, et al. (2014) Disturbances in melatonin secretion and circadian sleep–wake regulation in Parkinson disease. Sleep Med. 15: 342-347.
37. Mayeuf-Louchart A, Zecchin M, Staels B, Duez H (2017) Circadian control of metabolism and pathological consequences of clock perturbations. Biochimie 143: 42-50.
38. Reinke H, Asher G, (2016) Circadian clock control of liver metabolic functions. Gastroenterology 150: 574-580.
39. Ding G, et al. (2021) REV-ERB in GABAergic neurons controls diurnal hepatic insulin sensitivity. Nature 592: 763-767.
40. Marcheva B, et al. (2010) Disruption of the clock components CLOCK and BMAL1 leads to hypoinsulinaemia and diabetes. Nature 466: 627-631.
41. Pan X, Mota S, Zhang B, (2020) Circadian clock regulation on lipid metabolism and metabolic diseases. Adv. Exp. Med. Biol. 1276: 53-66.
42. Segers A, Depoortere I, (2021) Circadian clocks in the digestive system. Nat. Rev. Gastroenterol. Hepatol. 18: 239-251.
43. Ramsey KM, et al. (2009) Circadian clock feedback cycle through NAMPT-mediated NAD+ biosynthesis. Science 324: 651-654.
44. Chang H-C, Guarente L (2014) SIRT1 and other sirtuins in metabolism. Trends Endocrinol. Metab. 25: 138-145.
45. Asher G, et al. (2008) SIRT1 Regulates circadian clock gene expression through PER2 deacetylation. Cell 134: 317-328.
46. Liu L, Wang Z, Cao J, Dong Y, Chen Y (2019) Effect of melatonin on monochromatic light-induced changes in clock gene circadian expression in the chick liver. J. Photochem. Photobiol. B 197: 111537.
47. Powell EE, Wong VW-S, Rinella M (2021) Non-alcoholic fatty liver disease. Lancet 397: 2212-2224.
48. Joshi A, Upadhyay KK, Vohra A, Shirsath K, Devkar R, (2021) Melatonin induces Nrf2‐HO‐1 reprogramming and corrections in hepatic core clock oscillations in non‐alcoholic fatty liver disease. FASEB J. 35: e21803.
49. Stacchiotti A, et al. (2019) Melatonin effects on non-alcoholic fatty liver disease are related to microRNA-34a-5p/sirt1 axis and autophagy. Cells 8: 1053.
50. Chen J, et al. (2019) Protective effects of melatonin on sepsis-induced liver injury and dysregulation of gluconeogenesis in rats through activating SIRT1/STAT3 pathway. Biomed. Pharmacother. 117: 109150.
51. Xu S, et al. (2021) Melatonin attenuates sepsis-induced small-intestine injury by upregulating SIRT3-mediated oxidative-stress inhibition, mitochondrial protection, and autophagy induction. Front. Immunol. 12: 625627-625627.
52. Liu X-W, Wang C-D (2019) Melatonin alleviates circadian rhythm disruption exacerbating DSS-induced colitis by inhibiting the distribution of HMGB1 in intestinal tissues. Int. Immunopharmacol. 73: 108-117.
53. Kim SW, Kim S, Son M, Cheon JH, Park YS (2020) Melatonin controls microbiota in colitis by goblet cell differentiation and antimicrobial peptide production through Toll-like receptor 4 signalling. Sci. Rep. 10: 2232-2232.
54. Hong F, et al. (2020) Melatonin orchestrates lipid homeostasis through the hepatointestinal circadian clock and microbiota during constant light exposure. Cells 9: 489.
55. Xu L, et al. (2022) Suppression of obesity by melatonin through increasing energy expenditure and accelerating lipolysis in mice fed a high-fat diet. Nutr. Diabetes 12: 42.
56. Fernández Vázquez G, Reiter RJ, Agil A (2018) Melatonin increases brown adipose tissue mass and function in Zücker diabetic fatty rats: implications for obesity control. J. Pineal Res. 64: e12472.
57. Jiménez-Aranda A, et al. (2013) Melatonin induces browning of inguinal white adipose tissue in Zucker diabetic fatty rats. J. Pineal Res. 55: 416-423.
58. Stárka L, Dušková M (2020) What is a hormone? Physiol. Res. 69: S183-S185.
59. Głombik K, Detka J, Budziszewska B (2021) Hormonal regulation of oxidative phosphorylation in the brain in health and disease. Cells 10: 2937.
60. Gnocchi D, Bruscalupi G (2017) Circadian rhythms and hormonal homeostasis: pathophysiological implications. Biology (Basel) 6: 10.
61. Kim TW, Jeong J-H, Hong S-C (2015) The impact of sleep and circadian disturbance on hormones and metabolism. Int. J. Endocrinol. 2015: 591729-591729.
62. Serin Y, Acar Tek N (2019) Effect of circadian rhythm on metabolic processes and the regulation of energy balance. Ann. Nutr. Metab. 74: 322-330.
63. Gamble KL, Berry R, Frank SJ, Young ME (2014) Circadian clock control of endocrine factors. Nat. Rev. Endocrinol. 10: 466-475.
64. Jia S, Guo X, Chen Z, Li S, Liu X-A (2022) The roles of the circadian hormone melatonin in drug addiction. Pharmacol. Res. 183: 106371.
65. Boumans IJMM, de Boer IJM, Hofstede GJ, la Fleur SE., Bokkers EAM (2017) The importance of hormonal circadian rhythms in daily feeding patterns: An illustration with simulated pigs. Horm. Behav. 93: 82-93.
66. Liu X, et al. (2021) Mel1b and Mel1c melatonin receptors mediate green light-induced secretion of growth hormone in chick adenohypophysis cells via the AC/PKA and ERK1/2 signalling pathways. J. Photochem. Photobiol., B 225: 112322.
67. Zhu Q, et al. (2022) Melatonin inhibits testosterone synthesis in roosters Leydig cells by regulating lipolysis of lipid droplets. Theriogenology 189: 118-126.
68. Qin F, et al. (2015) Inhibitory effect of melatonin on testosterone synthesis is mediated via GATA-4/SF-1 transcription factors. Reprod. BioMed. Online 31: 638-646.
69. Deng S-L, et al. (2018) Melatonin promotes sheep Leydig cell testosterone secretion in a co-culture with Sertoli cells. Theriogenology 106: 170-177.
70. Ma J, et al. (2023) Effects of melatonin on development and hormone secretion of sheep theca cells in vitro. Theriogenology 198: 172-182.
71. Juszczak M, Boczek-Leszczyk E (2010) Hypothalamic gonadotropin-releasing hormone receptor activation stimulates oxytocin release from the rat hypothalamo-neurohypophysial system while melatonin inhibits this process. Brain Res. Bull. 81: 185-190.
72. Ghosh H, et al. (2022) Differential expression and interaction of melatonin and thyroid hormone receptors with estrogen receptor α improve ovarian functions in letrozole-induced rat polycystic ovary syndrome. Life Sci. 295: 120086.
73. Zhang J, et al. (2021) Melatonin alleviates the deterioration of oocytes and hormonal disorders from mice subjected to glyphosate. Mol. Cell. Endocrinol. 520: 111073.
74. Menéndez-Menéndez J, et al. (2019) Deciphering the molecular basis of melatonin protective effects on breast cells treated with doxorubicin: TWIST1 a transcription factor involved in EMT and metastasis, a novel target of melatonin. Cancers (Basel) 11: 1011.
75. Scheiermann C, Kunisaki Y, Frenette PS, (2013) Circadian control of the immune system. Nat. Rev. Immunol. 13: 190-198.
76. Pick R, He W, Chen C-S, Scheiermann C (2019) Time-of-day-dependent trafficking and function of leukocyte subsets. Trends Immunol. 40: 524-537.
77. Ackermann K, et al. (2012) Diurnal rhythms in blood cell populations and the effect of acute sleep deprivation in healthy young men. Sleep 35: 933-940.
78. Swanson KV, Deng M, Ting JPY (2019) The NLRP3 inflammasome: molecular activation and regulation to therapeutics. Nat. Rev. Immunol. 19: 477-489.
79. Liu T, Zhang L, Joo D, Sun S-C (2017) NF-κB signaling in inflammation. Signal Transduct. Target. Ther. 2: 17023.
80. Shen Y, et al. (2021) NF-κB modifies the mammalian circadian clock through interaction with the core clock protein BMAL1. PLoS Genet. 17: e1009933-e1009933.
81. Qin B, Deng Y (2015) Overexpression of circadian clock protein cryptochrome (CRY) 1 alleviates sleep deprivation-induced vascular inflammation in a mouse model. Immunol. Lett. 163: 76-83.
82. Ren D-l, et al. (2018) Circadian genes period1b and period2 differentially regulate inflammatory responses in zebrafish. Fish Shellfish Immunol. 77: 139-146.
83. Hergenhan S, Holtkamp S, Scheiermann C (2020) Molecular interactions between components of the circadian clock and the immune system. J. Mol. Biol. 432: 3700-3713.
84. Acuña-Fernández C, et al. (2020) Daily changes in the expression of clock genes in sepsis and their relation with sepsis outcome and urinary excretion of 6-sulfatoximelatonin. Shock 53: 550-559.
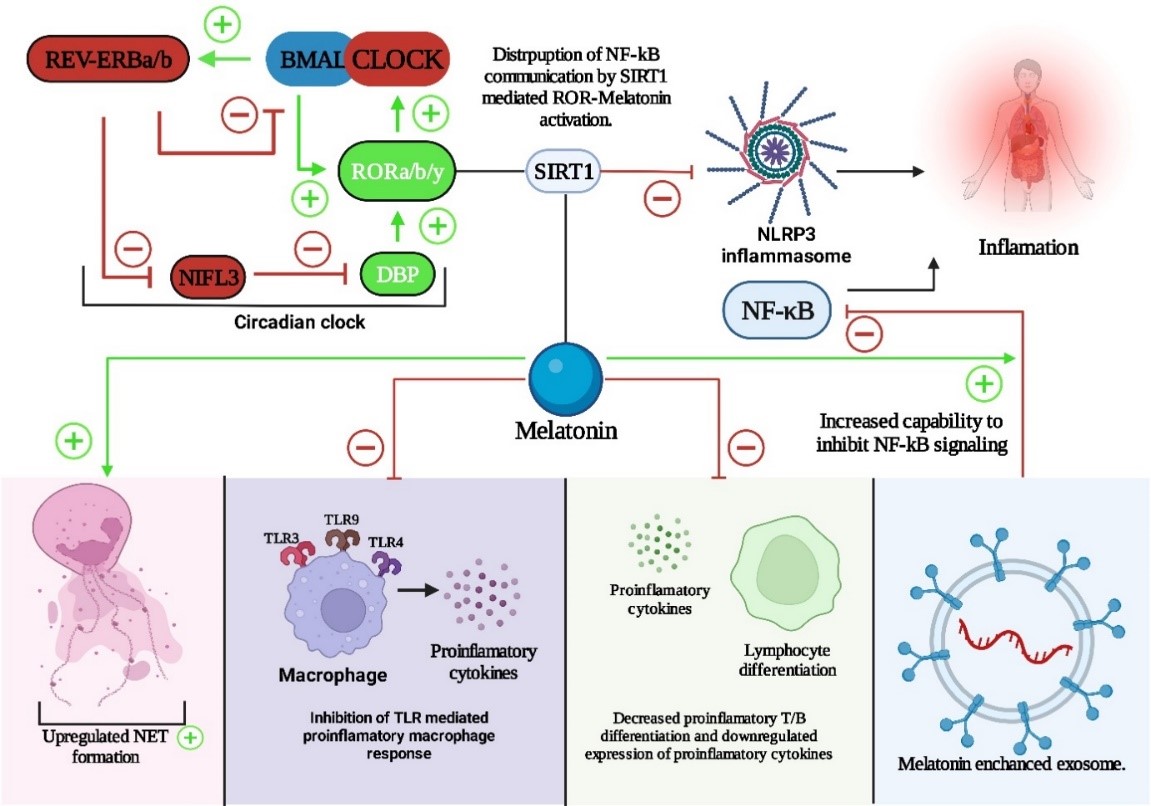
85. García JA, et al. (2015) Disruption of the NF-κB/NLRP3 connection by melatonin requires retinoid-related orphan receptor-α and blocks the septic response in mice. FASEB J. 29: 3863-3875.
86. Chibaatar E, Le K, Abdoulaye IA, Wu S, Guo Y (2020) Melatonin ameliorates lipopolysaccharide-induced microglial inflammation via triggering SIRT1/HMGB1 signaling axis. J. Mol. Neurosci. 71: 691-701.
87. Rahim I, et al. (2017) Melatonin administration to wild-type mice and nontreated NLRP3 mutant mice share similar inhibition of the inflammatory response during sepsis. J. Pineal Res. 63: e12410.
88. Xu L, et al. (2019) Protective effect of melatonin against polymicrobial sepsis is mediated by the anti-bacterial effect of neutrophils. Front. immunol. 10: 1371-1371.
89. Luo J, et al. (2020) Effect of melatonin on T/B cell activation and immune regulation in pinealectomy mice. Life Sci. 242: 117191.
90. Liu Y, Chen X-Q, Wang F, Cheng B, Zhou G (2022) Melatonin relieves Th17/CD4−CD8− T cells inflammatory responses via nuclear-receptor dependent manner in peripheral blood of primary Sjögren’s syndrome. Int. Immunopharmacol. 109: 108778.
91. Xu X, et al. (2018) Melatonin suppresses TLR9-triggered proinflammatory cytokine production in macrophages by inhibiting ERK1/2 and AKT activation. Sci. Rep. 8: 15579-15579.
92. Heo JS, Lim J-Y, Yoon DW, Pyo S, Kim J (2020) Exosome and melatonin additively attenuates inflammation by transferring miR-34a, miR-124, and miR-135b. Biomed. Res. Int. 2020: 1621394-1621394.
93. Wang K, et al. (2020) Melatonin enhances the therapeutic effect of plasma exosomes against cerebral ischemia-induced pyroptosis through the TLR4/NF-κB pathway. Front. Neurosci. 14: 848-848.
94. Farré-Alins V, et al. (2020) Melatonin reduces NLRP3 inflammasome activation by
increasing α7 nAChR-Mediated Autophagic Flux. Antioxidants (Basel) 9 (2020).

This work is licensed under a Creative Commons Attribution 4.0 International License.
For all articles published in Melatonin Res., copyright is retained by the authors. Articles are licensed under an open access Creative Commons CC BY 4.0 license, meaning that anyone may download and read the paper for free. In addition, the article may be reused and quoted provided that the original published version is cited. These conditions allow for maximum use and exposure of the work, while ensuring that the authors receive proper credit.
In exceptional circumstances articles may be licensed differently. If you have specific condition (such as one linked to funding) that does not allow this license, please mention this to the editorial office of the journal at submission. Exceptions will be granted at the discretion of the publisher.


