Potential therapeutic intervention of melatonin against COVID-19: A comparative pharmacokinetic study
Targets of melatonin in COVID-19
Abstract
Melatonin synthesis is primarily regulated by environmental light-dark cycle and is well known for its biological rhythm regulation and its potent antioxidant and anti-inflammatory properties across species. The present investigation focuses on the potential actions of melatonin as a therapeutic agent against COVID-19 and these actions are compared with other commonly used pharmacological agents of this kind including methylprednisolone, doxycycline, oseltamivir, and remdesivir. The comprehensive comparisons of pharmacokinetic profiles include their absorption, distribution, metabolism, and excretion (ADME) properties. The further in-depth analyses on their target identification, functional enrichment are performed by Gene Ontology (GO), Kyoto Encyclopedia of Genes and Genomes (KEGG) pathways, construction of protein-protein interaction (PPI) networks, and molecular docking. These analyses elucidate the potential correlation of melatonin with critical hub targets implicated in COVID-19 pathogenesis. The results from pharmacokinetics indicates that melatonin has the higher bioavailability than the other tested drugs due to its low molecular weight, lipophilicity, lack of P-glycoprotein (P-gp) along with inhibitory action on cytochrome P450 1A2 (CYP1A2). GO and enriched KEGG analyses suggests that melatonin-mediated modulation of COVID-19 pathogenesis likely targets the AGE-RAGE pathway, HIF-1α signaling, and apoptosis. Furthermore, PPI network analysis also shows that melatonin has the highest nodes and edges, as well as the greatest average node degree score and highest common potential targets with the genes associated with the development of COVID-19. Notably, molecular docking study demonstrates the substantial interactions of melatonin with principal hub targets TP53, AKT1, IL6, TNF, IL1B, BCL2, EGFR, STAT3, CASP3, and NFKB1. Hence, melatonin has several significant pharmacokinetic advantages compared to selected therapeutic agents which may appear to modulate multiple facets of COVID-19 pathology. Based on the significant pharmacokinetic advantages of melatonin over the commonly used other drugs, the substantial clinical studies are necessary to establish its methods of application as a potential therapeutic against SARS-CoV-2 in the near future.
References
2. Hikmet F, Méar L, Edvinsson Å, Micke P, Uhlén M, Lindskog C (2020) The protein expression profile of ACE2 in human tissues. Mol. Syst. Biol. 16: e9610. doi:10.15252/msb.20209610.
3. Bourgonje AR, Abdulle AE, Timens W, Hillebrands JL, Navis GJ, Gordijn SJ, Bolling MC, Dijkstra G, Voors AA, Osterhaus AD, van der Voort PH, Mulder DJ, van Goor H (2020) Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19). J. Pathol. 251: 228-248. doi:10.1002/path.5471.
4. Clay C, Donart N, Fomukong N, Knight JB, Lei W, Price L, Hahn F, Westrienen JV, Harrod KS (2012) Primary severe acute respiratory syndrome coronavirus infection limits replication but not lung inflammation upon homologous rechallenge. J. Virol. 86: 4234-4244. doi:10.1128/JVI.06791-11.
5. Diao B, Wang C, Tan Y, Chen X, Liu Y, Ning L, Chen L, Li M, Liu Y, Wang G, Yuan Z, Feng Z, Wu Y, Chen Y (2020) Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019 (COVID-19). Front. Immunol. 11: 827. doi:10.3389/fimmu.2020.00827.
6. Huo C, Xiao K, Zhang S, Tang Y, Wang M, Qi P, Xiao J, Tian H, Hu Y (2018) H5N1 influenza a virus replicates productively in pancreatic cells and induces apoptosis and pro-inflammatory cytokine response. Front. Cell Infect. Microbiol. 8: 386. doi:10.3389/fcimb.2018.00386.
7. Chaudhary N, Weissman D, Whitehead KA (2021) mRNA vaccines for infectious diseases: principles, delivery and clinical translation. Nat. Rev. Drug Discov. 20: 817-838. doi:10.1038/s41573-021-00283-5.
8. Dolgin E (2022) Pan-coronavirus vaccine pipeline takes form. Nat. Rev. Drug Discov. 21: 324-326. doi:10.1038/d41573-022-00074-6.
9. Meganck RM, Baric RS (2021) Developing therapeutic approaches for twenty-first-century emerging infectious viral diseases. Nat. Med. 27: 401-410. doi:10.1038/s41591-021-01282-0.
10. Wang M, Cao R, Zhang L, Yang X, Liu J, Xu M, Shi Z, Hu Z, Zhong W, Xiao G (2020) Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 30: 269-271. doi:10.1038/s41422-020-0282-0.
11. Li G, Hilgenfeld R, Whitley R, Clercq ED (2023) Therapeutic strategies for COVID-19: progress and lessons learned. Nat. Rev. Drug Discov. 22: 449-475. doi:10.1038/s41573-023-00672-y.
12. Hayden FG, Treanor JJ, Fritz RS, Lobo M, Betts RF, Miller M, Kinnersley N, Mills RG, Ward P, Straus SE (1999) Use of the oral neuraminidase inhibitor oseltamivir in experimental human influenza: randomized controlled trials for prevention and treatment. JAMA. 282:1240-1246. doi:10.1001/jama.282.13.1240.
13. Tan Q, Duan L, Ma Y, Wu F, Huang Q, Mao K, Xiao W, Xia H, Zhang S, Zhou E, Ma P, Song S, Li Y, Zhao Z, Sun Y, Li Z, Geng W, Yin Z, Jin Y (2020) Is oseltamivir suitable for fighting against COVID-19: In silico assessment, in vitro and retrospective study. Bioorg. Chem. 104: 104257. doi:10.1016/j.bioorg.2020.104257.
14. Chiba S (2021) Effect of early oseltamivir on outpatients without hypoxia with suspected COVID-19. Wien Klin Wochenschr. 133: 292-297. doi:10.1007/s00508-020-01780-0.
15. Li G, Yue T, Zhang P, Gu W, Gao L, Tan L (2021) Drug discovery of nucleos(t)ide antiviral agents. Molecules 26: 923. doi:10.3390/molecules26040923.
16. Hardy RS, Raza K, Cooper MS (2020) Therapeutic glucocorticoids: mechanisms of actions in rheumatic diseases. Nat. Rev. Rheumatol. 16: 133-144. doi:10.1038/s41584-020-0371-y.
17. Hazbun ME, Faust AC, Ortegon AL, Sheperd LA, Weinstein GL, Doebele RL, Weinmeister KD, Liddell AM, Feldman M (2020) The combination of tocilizumab and methylprednisolone along with initial lung recruitment strategy in coronavirus disease 2019 patients requiring mechanical ventilation: A series of 21 consecutive cases. Crit. Care Explor. 2: e0145. doi:10.1097/CCE.0000000000000145.
18. Yates PA, Newman SA, Oshry LJ, Glassman RH, Leone AM, Reichel E (2020) Doxycycline treatment of high-risk COVID-19-positive patients with comorbid pulmonary disease. Ther. Adv. Respir. Dis. 14: 1753466620951053. doi:10.1177/1753466620951053.
19. Reiter RJ, Abreu-Gonzalez P, Marik PE, Dominguez-Rodriguez A (2020) Therapeutic algorithm for use of melatonin in patients with COVID-19. Front. Med. (Lausanne). 7: 226. doi:10.3389/fmed.2020.00226.
20. Zhang R, Wang X, Ni L, Di X, Ma B, Niu S, Liu C, Reiter RJ (2020) COVID-19: Melatonin as a potential adjuvant treatment. Life Sci. 250: 117583. doi:10.1016/j.lfs.2020.117583.
21. Chacin-Bonilla L, Bonilla E (2024) Melatonin and viral infections: A review focusing on therapeutic effects and SARS-CoV-2. Melatonin Res. 7: 47-83. doi: 10.32794/mr112500168.
22. Chavarría AP, Vázquez RRV, Cherit JGD, Bello HH, Suastegui HC, Moreno-Castañeda L, Estrada GA, Hernández F, González-Marcos O, Saucedo-Orozco H, Manzano-Pech L, Márquez-Velasco R, Guarner-Lans V, Pérez-Torres I, Soto ME (2021) Antioxidants and pentoxifylline as coadjuvant measures to standard therapy to improve prognosis of patients with pneumonia by COVID-19. Comput. Struct. Biotechnol. J. 19: 1379-1390. doi:10.1016/j.csbj.2021.02.009.
23. Esmaeili Gouvarchin Ghaleh H, Hosseini A, Aghamollaei H, Fasihi-Ramandi M, Alishiri G, Saeedi-Boroujeni A, Hassanpour K, Mahmoudian-Sani M, Farnoosh G (2021) NLRP3 inflammasome activation and oxidative stress status in the mild and moderate SARS-CoV-2 infected patients: impact of melatonin as a medicinal supplement. Z. Naturforsch. C. J. Biosci. 77: 37-42. doi:10.1515/znc-2021-0101.
24. Hosseini A, Esmaeili Gouvarchin Ghaleh H, Aghamollaei H, Ramandi MF, Alishiri G, Shahriary A, Hassanpour K, Tat M, Farnoosh G (2021) Evaluation of Th1 and Th2 mediated cellular and humoral immunity in patients with COVID-19 following the use of melatonin as an adjunctive treatment. Eur. J. Pharmacol. 904: 174193. doi:10.1016/j.ejphar.2021.174193.
25. Hasan ZT, Atrakji MQYMAA, Mehuaiden AK (2022) The effect of melatonin on thrombosis, sepsis and mortality rate in COVID-19 patients. Int. J. Infect. Dis. 114: 79-84. doi:10.1016/j.ijid.2021.10.012.
26. Chacin-Bonilla L, Bonilla E (2024) Multiple actions of melatonin in reducing viral pathophysiologies. Melatonin Res. 7: 153-180. doi: 10.32794/mr112500173.
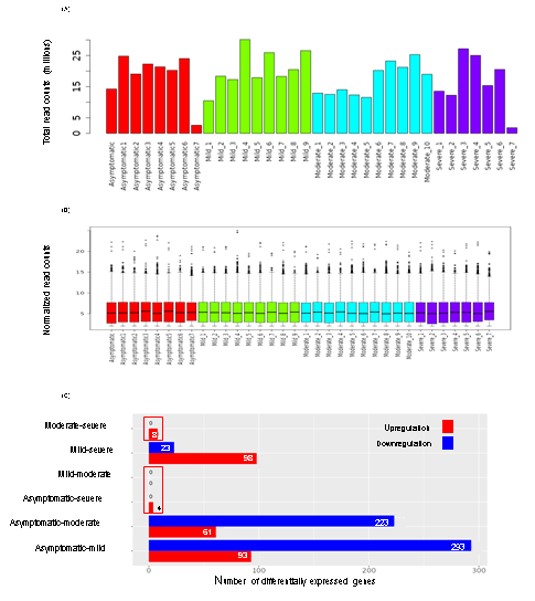
27. Ge SX, Son EW, Yao R (2018) iDEP: an integrated web application for differential expression and pathway analysis of RNA-Seq data. BMC Bioinformatics 19: 534. doi:10.1186/s12859-018-2486-6.
28. Daina A, Michielin O, Zoete V (2017) SwissADME: a free web tool to evaluate pharmacokinetics, drug-likeness and medicinal chemistry friendliness of small molecules. Sci. Rep. 7: 42717. doi:10.1038/srep42717.
29. Acharyya A, Das J, Hasan KN (2023) In silico study to unravel molecular networking of melatonin in the regulation of gametogenesis. J. Mol. Endocrinol. 71: e230053. doi:10.1530/JME-23-0053.
30. Acharyya A, Das J, Hasan KN (2023) Rhythmicity in testicular melatonin and its correlation with the dynamics of spermatogenic cells in an annual reproductive cycle of Clarias batrachus under natural photo-thermal conditions. Theriogenology 208: 15-27. doi:10.1016/j.theriogenology.2023.06.001.
31. Hu Q, Feng M, Lai L, Pei J (2018) Prediction of drug-likeness using deep autoencoder neural networks. Front. Genet. 9: 585. doi:10.3389/fgene.2018.00585.
32. Lobo S (2020) Is there enough focus on lipophilicity in drug discovery? Expert. Opi. Drug Discov. 15: 261-263. doi: 10.1080/17460441.2020.1691995.
33. Finch A, Pillans P (2014) P-glycoprotein and its role in drug-drug interactions. Aust. Prescr. 37: 137-139. doi:10.18773/austprescr.2014.050.
34. Chang TK, Chen J, Yang G, Yeung EY (2010) Inhibition of procarcinogen-bioactivating human CYP1A1, CYP1A2 and CYP1B1 enzymes by melatonin. J. Pineal Res. 48: 55-64. doi:10.1111/j.1600-079X.2009.00724.x.
35. Saini S, Saini A, Thakur CJ, Kumar V, Gupta RD, Sharma JK (2020) Genome-wide computational prediction of miRNAs in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) revealed target genes involved in pulmonary vasculature and antiviral innate immunity. Mol. Biol. Res. Commun. 9: 83-91. doi:10.22099/mbrc.2020.36507.1487.
36. Ma-Lauer Y, Carbajo-Lozoya J, Hein MY, Müller MA, Deng W, Lei J, Meyer B, Kusov Y, von Brunn B, Bairad DR, Hünten S, Drosten C, Hermeking H, Leonhardt H, Mann M, Hilgenfeld R, von Brunn A (2016) p53 down-regulates SARS coronavirus replication and is targeted by the SARS-unique domain and PLpro via E3 ubiquitin ligase RCHY1. Proc. Natl. Acad. Sci. USA. 113: E5192-E5201. doi:10.1073/pnas.1603435113.
37. Klein AM, de Queiroz RM, Venkatesh D, Prives C (2021) The roles and regulation of MDM2 and MDMX: it is not just about p53. Genes Dev. 35: 575-601. doi:10.1101/gad.347872.120.
38. Zauli G, Tisato V, Secchiero P (2020) Rationale for considering oral Idasanutlin as a therapeutic option for COVID-19 patients. Front. Pharmacol. 11: 1156. doi:10.3389/fphar.2020.01156.
39. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395: 497-506. doi:10.1016/S0140-6736(20)30183-5.
40. Cohen MM Jr (2013) The AKT genes and their roles in various disorders. Am. J. Med. Genet. A. 161: 2931-2937. doi:10.1002/ajmg.a.36101.
41. Xia QD, Xun Y, Lu JL, Lu YC, Yang YY, Zhou P, Hu J, Li C, Wang S (2020) Network pharmacology and molecular docking analyses on Lianhua Qingwen capsule indicate Akt1 is a potential target to treat and prevent COVID-19. Cell Prolif. 53: e12949. doi:10.1111/cpr.12949.
42. Wang X, Zhang H, Abel AM, Young AJ, Xie L, Xie Z (2014) Role of phosphatidylinositol 3-kinase (PI3K) and Akt1 kinase in porcine reproductive and respiratory syndrome virus (PRRSV) replication. Arch. Virol. 159: 2091-2096. doi:10.1007/s00705-014-2016-4.
43. Que Y, Hu C, Wan K, Hu P, Wang R, Luo J, Li T, Ping R, Hu Q, Sun Y, Wu X, Tu L, Du Y, Chang C, Xu G (2022) Cytokine release syndrome in COVID-19: a major mechanism of morbidity and mortality. Int. Rev. Immunol. 41: 217-230. doi:10.1080/08830185.2021.1884248.
44. Hu S, Li Z, Chen X, Liang CH (2021) Computed tomography manifestations in super early stage 2019 novel coronavirus pneumonia. Acta Radiol. 62: 360-367. doi:10.1177/0284185120924806.
45. Lagunas-Rangel FA, Chávez-Valencia V (2020) High IL-6/IFN-γ ratio could be associated with severe disease in COVID-19 patients. J. Med. Virol. 92: 1789-1790. doi:10.1002/jmv.25900.
46. Jang DI, Lee AH, Shin HY, Song HR, Park JH, Kang TB, Lee SR, Yang SH (2021) The Role of tumor necrosis factor alpha (TNF-α) in autoimmune disease and current TNF-α inhibitors in therapeutics. Int. J. Mol. Sci. 22: 2719. doi:10.3390/ijms22052719.
47. Dong G, Wang F, Xu L, Zhu M, Zhang B, Wang B (2019) Serum interleukin-18: A novel prognostic indicator for acute respiratory distress syndrome. Medicine (Baltimore). 98: e15529. doi:10.1097/MD.0000000000015529.
48. Bartolini D, Stabile AM, Vacca C, Pistilli A, Rende M, Gioiello A, Cruciani G, Galli F (2022) Endoplasmic reticulum stress and NF-kB activation in SARS-CoV-2 infected cells and their response to antiviral therapy. IUBMB Life 74: 93-100. doi:10.1002/iub.2537.
49. Hariharan A, Hakeem AR, Radhakrishnan S, Reddy MS, Rela M (2021) The role and therapeutic potential of NF-kappa-B pathway in severe COVID-19 patients. Inflammopharmacol. 29: 91-100. doi:10.1007/s10787-020-00773-9.
50. Cheng F, Rao S, Mehra R (2020) COVID-19 treatment: Combining anti-inflammatory and antiviral therapeutics using a network-based approach. Cleve. Clin. J. Med. doi:10.3949/ccjm.87a.ccc037.
51. Terpos E, Ntanasis-Stathopoulos I, Elalamy I, Kastritis E, Sergentanis TN, Politou M, Psaltopoulou T, Gerotziafas G, Dimopoulos MA (2020) Hematological findings and complications of COVID-19. Am. J. Hematol. 95: 834-847. doi:10.1002/ajh.25829.
52. Aslam M, Ladilov Y (2020) Targeting the sAC-dependent cAMP pool to prevent SARS-Cov-2 Infection. Cells. 9: 1962. doi:10.3390/cells9091962.
53. Man SM, Karki R, Kanneganti TD (2017) Molecular mechanisms and functions of pyroptosis, inflammatory caspases and inflammasomes in infectious diseases. Immunol. Rev. 277: 61-75. doi:10.1111/imr.12534.
54. McMahon CL, Staples H, Gazi M, Carrion R, Hsieh J (2021) SARS-CoV-2 targets glial cells in human cortical organoids. Stem Cell Reports 16: 1156-1164. doi:10.1016/j.stemcr.2021.01.016.
55. Premeaux TA, Yeung ST, Bukhari Z, Bowler S, Alpan O, Gupta R, Ndhlovu LC (2022) Emerging insights on caspases in COVID-19 pathogenesis, sequelae, and directed therapies. Front. Immunol. 13: 842740. doi:10.3389/fimmu.2022.842740.
56. Camp OG, Bai D, Gonullu DC, Nayak N, Abu-Soud HM (2021) Melatonin interferes with COVID-19 at several distinct ROS-related steps. J. Inorg. Biochem. 223: 111546. doi:10.1016/j.jinorgbio.2021.111546.
57. Hatabu H, Kaye KM, Christiani DC (2023) Viral infection, pulmonary fibrosis, and long COVID. Am. J. Respir. Crit. Care Med. 207: 647-649. doi:10.1164/rccm.202211-2121ED.
58. Bhatia R, Gautam SK, Cannon A, Thompson C, Hall BR, Aithal A, Banerjee K, Jain M, Solheim JC, Kumar S, Batra SK (2019) Cancer-associated mucins: role in immune modulation and metastasis. Cancer Metastasis Rev. 38: 223-236. doi:10.1007/s10555-018-09775-0.
59. Engler M, Albers D, Von Maltitz P, Groß R, Münch J, Cirstea IC (2023) ACE2-EGFR-MAPK signaling contributes to SARS-CoV-2 infection. Life Sci. Alliance 6: e202201880. doi:10.26508/lsa.202201880.
60. Jafarzadeh A, Nemati M, Jafarzadeh S (2021) Contribution of STAT3 to the pathogenesis of COVID-19. Microb. Pathog. 154: 104836. doi:10.1016/j.micpath.2021.104836.
61. Huang PY, Wu JY, Liu TH, Tsai YW, Chen PT, Liao CT, Toh HS (2023) The clinical efficacy of melatonin in the treatment of patients with COVID-19: a systematic review and meta-analysis of randomized controlled trials. Front. Med. 10: 1171294. doi: 10.3389/fmed.2023.1171294.
62. Ganjifarda M, Ghafarib S, Sahebnasaghc A, Esmaeilid M, Amirabadizadehe AR, Ebrahimzadehf A, Askarif P, Avan R (2024) Evaluation of the effect of melatonin on patients with COVID-19 admitted to ICU: A double-blind randomized clinical trial. Vacunas. doi: 10.1016/j.vacun.2024.09.004 (In press).
63. Molina-Carballo A, Jerez-Calero A, Fernández-López L, Augustin-Morales M del C, Muñoz-Hoyos A, Agil A (2023) The preventive and protective role of melatonin in SARS-CoV-2 infection: a retrospective study. Melatonin Res. 6: 372-396. doi:10.32794/mr112500159.
64. Tan DX, Reiter RJ (2022) Mechanisms and clinical evidence to support melatonin's use in severe COVID-19 patients to lower mortality. Life Sci. 294:120368. doi: 10.1016/j.lfs.2022.120368.

This work is licensed under a Creative Commons Attribution 4.0 International License.
For all articles published in Melatonin Res., copyright is retained by the authors. Articles are licensed under an open access Creative Commons CC BY 4.0 license, meaning that anyone may download and read the paper for free. In addition, the article may be reused and quoted provided that the original published version is cited. These conditions allow for maximum use and exposure of the work, while ensuring that the authors receive proper credit.
In exceptional circumstances articles may be licensed differently. If you have specific condition (such as one linked to funding) that does not allow this license, please mention this to the editorial office of the journal at submission. Exceptions will be granted at the discretion of the publisher.


