A geographical approach to the development of hypotheses relating to Covid-19 death rates
Geography of Covid-19 death rates, developing hypotheses
Abstract
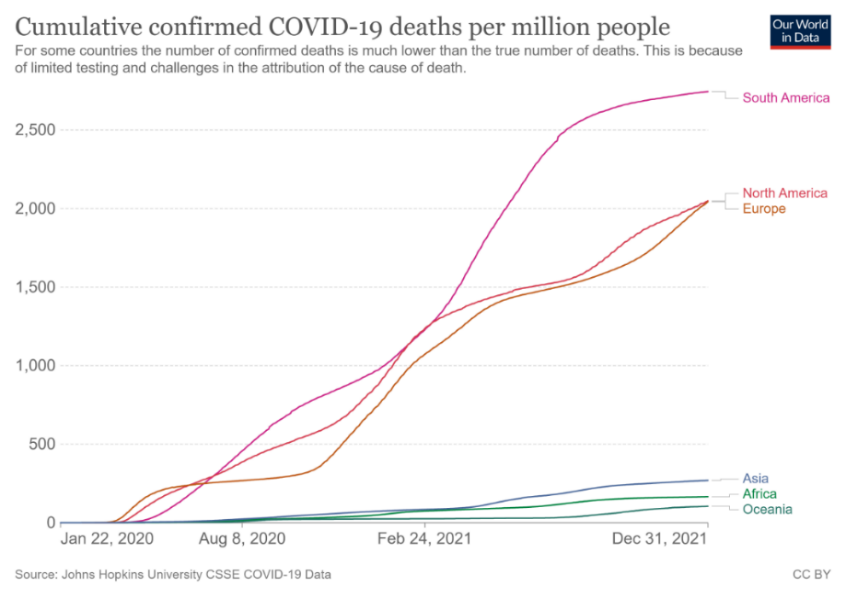
Covid-19 deaths per million vary greatly between continents, with countries in South America having higher death rates even than Europe and North America, while Asia, Africa and Oceania have death rates which are only a fifth of those in South America. By analysing national level data on body weight, diet and latitude, we hypothesise and demonstrate that difference in the percentage of people with overweight (BMI > 25) may be the major factor that explains these differences in Covid-19 death rates. Meanwhile, within the group of countries where adult overweight is prevalent (i.e., where more than 50% of the population has BMI > 25), we hypothesise and demonstrate that latitude plays a role, with relatively lower death rates occurring in countries at lower latitudes. We further suggest that these relationships may be explained by two possible medical hypotheses relating to solar radiation: (1) In overweight people there is less penetration to important organs of near-infrared radiation (NIR) which stimulates production of subcellular melatonin, a strong anti-oxidizing factor and (2) In overweight people, fatty tissue holds much of the body´s 25(OH)D3 leaving less circulating in the blood stream. Several pathways have been proposed by other researchers to explain the link between Vitamin D deficiency and severity of Covid-19, but the possible link of Covid-19 outcome with NIR has not been explored. Latitude, of course, determines the amount of incoming NIR and as well as UV-B, which is the main stimulant for the body´s production of Vitamin D. It may well be that these two physiological processes operate simultaneously.
References
2. UN Dept. of Economic and Social Affairs, Population Division (2019). World Population Prospects. https://population.un.org/wpp/#:~:text=The%202019%20Revision%20of%20World,of%20the%20United%20Nations%20Secretariat.
3. Daneshkhah A, Eshein A, Subramanian H, Roy HK, Backman V (2020) The role of vitamin D in suppressing cytokine storm in COVID-19 Patients and Associated Mortality. medRxiv. preprint doi: https://doi.org/10.1101/2020.04.08.20058578.
4. Davies G, Garami AR, Byers JC (2020) COVID-19 and vitamin D information. medRxiv. https://docs.google.com/document/d/1jffdZOSuIA64L_Eur8qyCQ12T7NXrHSKPxtMe134C0Y/edit.
5. Grant WB, Lahore H, McDonnell SL, Baggerly CA, French CB, Aliano JL, Bhattoa HP (2020) Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients 12 (4): 988-1007.
6. Greiller CL, Martineau AR (2015) Modulation of the immune response to respiratory viruses by vitamin D. Nutrients 7 (6): 4240-4270.
7. Ilie PC, Stefanescu S, Smith L (2020) The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality. Aging. Clin. Exp. Res. 32 (7): 1195-1198.
8. Laird E, Rhodes J, Kenny RA (2020) Vitamin D and inflammation: potential implications for severity of COVID-19. Irish Med. J. 113 (5): 81-88.
9. Pugach IZ, Pugach S (2020) Strong correlation between prevalence of severe vitamin d deficiency and population mortality rate from COVID-19 in Europe. Wiener Klinische Wochenschrift 133: 403-405.
10. Radjukovic A, Hippchen T, Tiwari-Heckler S, Dreher S, Boxberger M, Merle, U (2020) Vitamin D deficiency and outcome of COVID-19 patients. Nutrients 12: 2757.
11. Rodríguez TA, Montelongo MEA, Martinez-Cuazitl A, Puente NAV, Reyes P (2020) Deficiency of Vitamin D is a risk factor of mortality in patients with COVID-19. Revista de Sanidad Militar 74: 1-2.
12. WOF (World Obesity Federation) (2021) COVID-19 and Obesity: The 2021 Atlas. www.worldobesity.org.
13. WHO Global Health Observatory (2020) https://apps.who.int/gho/data/view.main.CTRY2430A.
14. Food and Agriculture Organization, FAOSTAT Food Balance Sheets 2014-2017. http://www.fao.org/faostat/en/#data/FBS.
15. Saji, B. (nd) In-depth intuition of K-means clustering algorithm in machine learning. Analytics Vidhya, https://www.analyticsvidhya.com/blog/2021/01/in-depth-intuition-of-k-means-clustering-algorithm-in-machine-learning/ Consulted 2/2/2022.
16. UC Business Analytics (nd) K-means cluster analysis. https://uc-r.github.io/kmeans_clustering Consulted 2/2/2022.
17. Gao M, Piernas C, Astbury NM, Hippisley-Cox J, O'Rahilly S, Aveyard P, Jebb SA (2021) Associations between body-mass index and COVID-19 severity in 6·9 million people in England: a prospective, community-based, cohort study. Lancet Diabetes Endocrinol. 9 (6): 350-359.
18. New York Times Apple Podcast (April 7 2022) The Covid mystery in Africa. https://podcasts.apple.com/us/podcast/the-daily6/id1200361736?i=1000556512333.
19. Baak, van MA, Astrup A (2009) Consumption of sugars and body weight. Obes. Rev. 10: 9-23.
20. Olsen NJ, Andersen LB, Wedderkopp N, Kristensen PL, Heitmann BL (2012) Intake of liquid and solid sucrose in relation to changes in body fatness over 6 years among 8-to 10-year-old children: the European Youth Heart Study. Obes. Facts 5 (4): 506-512.
21. Wang J, Light K, Henderson M, O'Loughlin J, Mathieu ME, Paradis G, Gray-Donald K (2014) Consumption of added sugars from liquid but not solid sources predicts impaired glucose homeostasis and insulin resistance among youth at risk of obesity. J. Nutrition 144 (1): 81-86.
22. Sundborn G, Thornley S, Merriman TR, Lang B, King C, Lanaspa MA, Johnson RJ (2019) Are liquid sugars different from solid sugar in their ability to cause metabolic syndrome? Obesity 27 (6): 879-887.
23. Walrand S. (2021) Autumn COVID-19 surge dates in Europe correlated to latitudes, not to temperature-humidity, pointing to vitamin D as contributing factor. Sci. Rep. 11 (1): 1-9.
24. Schuit M, Gardner S, Wood S, Bower K, Williams G, Freeburger D, Dabisch P (2020) The influence of simulated sunlight on the inactivation of influenza virus in aerosols. J. Infect. Dis. 221 (3): 372-378.
25. Kwok RM, Torres DM, Harrison SA (2013) Vitamin D and non-alcoholic fatty liver disease (NAFLD): is it more than just an association? Hepatology 58 (3): 1166-1174.
26. Cordeiro A, Pereira S, Saboya CJ, Ramalho A (2017) Relationship between non-alcoholic fatty liver disease and vitamin D nutritional status in extreme obesity. Can. J. Gastroenterol. Hepatol. 9456897: 1-8.
27. Borges-Canha M, Neves JS, Mendonça F, Silva MM, Costa C, Cabral PM, Guerreiro V, Lourenço R, Meira P, Salazar D, Ferreira MJ (2021) The impact of vitamin D in non-alcoholic fatty liver disease: a cross-sectional study in patients with morbid obesity. Diabetes Metab. Syndr. Obes. 14: 487-495.
28. Eliades M, Spyrou E, Agrawal N, Lazo M, Brancati FL, Potter JJ, Koteish AA, Clark JM, Guallar E, Hernaez R (2013) Meta‐analysis: vitamin D and non‐alcoholic fatty liver disease. Aliment. Pharmacol. Ther. 38 (3): 246-254.
29. Arjmand AT, Jafarian S (2018) Time for a U-turn on understanding the major cause of universal human hypovitaminosis D. Ann. Clin. Lab. Res. 6 (2): 1-4.
30. Benskin LL (2020) A basic review of the preliminary evidence that COVID-19 risk and severity is increased in vitamin D deficiency. Front. Public Health 8: 513, 1-25.
31. Crafa A, Cannarella R, Condorelli RA, Mongioì LM, Barbagallo F, Aversa A, La Vignera S, Calogero AE (2021) Influence of 25-hydroxy-cholecalciferol levels on SARS-CoV-2 infection and COVID-19 severity: A systematic review and meta-analysis. EClinicalMedicine 37: 100967.
32. Borsche L, Glauner B Mendel JV (2021) COVID-19 mortality risk correlates inversely with vitamin D3 status, and a mortality rate close to zero could theoretically be achieved at 50 ng/ml 25 (OH) D3: Results of a systematic review and meta-analysis. Nutrients 13 (10): 3596.
33. Wang TT, Nestel FP, Bourdeau V, Nagai Y, Wang Q, Liao J, Tavera-Mendoza L, Lin R, Hanrahan JW, Mader S, White JH (2004) Cutting edge: 1, 25-dihydroxyvitamin D3 is a direct inducer of antimicrobial peptide gene expression. J. Immunol. 173 (5): 2909-2912.
34. Kota S, Sabbah A, Harnack R, Xiang Y, Meng X, Bose S (2008) Role of human β-defensin-2 during tumor necrosis factor-α/NF-κB-mediated innate antiviral response against human respiratory syncytial virus. J. Biol. Chem. 283 (33): 22417-22429.
35. Currie SM, Findlay EG, McHugh BJ, Mackellar A, Man T, Macmillan D, Wang H, Fitch PM, Schwarze J, Davidson DJ (2013) The human cathelicidin LL-37 has antiviral activity against respiratory syncytial virus. PloS One 8 (8): e73659.
36. Zdrenghea MT, Makrinioti H, Bagacean C, Bush A, Johnston SL, Stanciu LA (2017) Vitamin D modulation of innate immune responses to respiratory viral infections. Rev. Med. Virol. 27 (1): 1909.
37. van de Veerdonk FL, Netea MG, van Deuren M, van der Meer JW, de Mast Q, Brüggemann RJ, van der Hoeven H (2020) Kallikrein-kinin blockade in patients with COVID-19 to prevent acute respiratory distress syndrome. Elife 9: e57555.
38. Heras de las N, Martín Giménez VM, Ferder L, Manucha W, Lahera V (2020) Implications of oxidative stress and potential role of mitochondrial dysfunction in COVID-19: therapeutic effects of vitamin D. Antioxidants 9 (9): 897.
39. Cherrie M, Clemens T, Colandrea C, Feng Z, Webb DJ, Weller RB, Dibben C (2021) Ultraviolet A radiation and COVID-19 deaths in the USA with replication studies in England and Italy. Br. J. Dermatol. 185 (2): 363-370.
40. Zimmerman S, Reiter RJ (2019) Melatonin and the optics of the human body. Melatonin Res. 2 (1): 138-160.
41. Schönrich G, Raftery MJ, Samstag Y (2020) Devilishly radical NETwork in COVID-19: Oxidative stress, neutrophil extracellular traps (NETs), and T cell suppression. Adv. Biol. Regul. 77: 100741.
42. Laforge M, Elbim C, Frère C, Hémadi M, Massaad C, Nuss P, Benoliel JJ, Becker C (2020) Tissue damage from neutrophil-induced oxidative stress in COVID-19. Nat. Rev. Immunol. 20 (9): 515-516.

This work is licensed under a Creative Commons Attribution 4.0 International License.
For all articles published in Melatonin Res., copyright is retained by the authors. Articles are licensed under an open access Creative Commons CC BY 4.0 license, meaning that anyone may download and read the paper for free. In addition, the article may be reused and quoted provided that the original published version is cited. These conditions allow for maximum use and exposure of the work, while ensuring that the authors receive proper credit.
In exceptional circumstances articles may be licensed differently. If you have specific condition (such as one linked to funding) that does not allow this license, please mention this to the editorial office of the journal at submission. Exceptions will be granted at the discretion of the publisher.


