Melatonin and redox homeostasis
Melatonin and redox homeostasis
Abstract
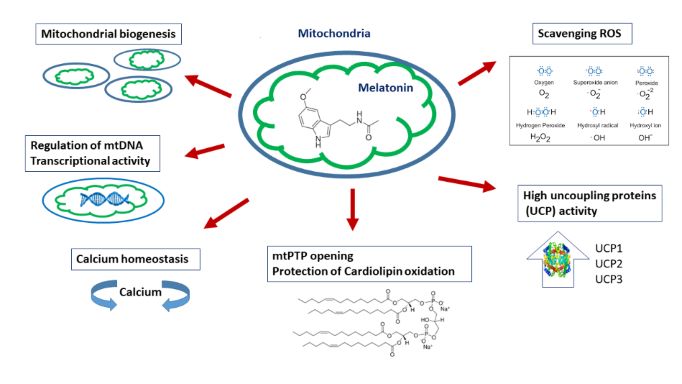
Redox homeostasis and redox signaling are constituents of preservation of a normal physiological state. Whereas the equilibrium between oxidants and nucleophiles is conserved in redox homeostasis, oxidative stress promotes the formation of a radically altered redox state. It is known that modification of circadian clock may lead to severe alteration in redox balance. Melatonin [N-acetyl-5-methoxytryptamine, (MLT)] regulates numerous physiological functions including circadian rhythm, sleep-wake cycle, gonadal activity, redox homeostasis, neuroprotection, immune-modulation, and anticancer activity in organisms. Insufficient MLT production is closely related to development of aging process, tumorigenesis, visceral adiposity, neurodegenerative disorders, etc. Reactive oxygen species (ROS) are not intrinsically harmful or beneficial in cellular redox metabolism. Redox homeostasis is an integrative status for both of the hormetic response to ROS overproduction and subsequent redox signaling. MLT and its derivatives are traditionally classified as hormone-like substances. Their redox sensitive regulatory activity and direct interaction with intracellular ROS serve as second messenger in cell signaling. This review involves the role of redox homeostasis in the pathogenesis of age-related disorders and its relationship with MLT, therefore, targeting the circadian rhythm may propose new therapeutic approach for these disorders.
References
2. Yanar K, Simsek B, Çakatay U (2019) Integration of oxidative related redox homeostasis, aging, and circadian rhythm. Rejuvenation Res. 22 (5): 409-419.
3. Jiang J, et al. (2021) Melatonin ameliorates PM2.5 -induced cardiac perivascular fibrosis through regulating mitochondrial redox homeostasis. J. Pineal Res. 70 (1): e12686.
4. Reiter RJ, Tan DX, Fuentes-Broto L (2010) Melatonin: a multitasking molecule. Prog. Brain Res. 181: 127-51.
5. Zisapel N (2018) New perspectives on the role of melatonin in human sleep, circadian rhythms and their regulation. Br. J. Pharmacol. 175 (16): 3190–3199.
6. Hardeland R (2009) Melatonin signaling mechanisms of a pleiotropic agent. Biofactors 35 (2): 183-192.
7. Acuna-Castroviejo D, et al. (2002) Melatonin, mitochondrial homeostasis and mitochondrial-related diseases. Curr. Top. Med. Chem. 2: 133-151.
8. Samanta S (2020) Melatonin: an endogenous miraculous indolamine, fights against cancer progression. J. Cancer Res. Clin. Oncol. 146 (8): 1893-1922.
9. Hardeland R, Pandi-Perumal SR (2002) Melatonin, a potent agent in antioxidative defense: actions as a natural food constituent, gastrointestinal factor, drug and prodrug. Nutr. Metab. (Lond) 2: 22.
10. Zhang, H-M, Zhang, Y (2014) Melatonin: a well-documented antioxidant with conditional pro-oxidant actions. J. Pineal Res. 57 (2): 131-146.
11. Zisapel N (2010) Melatonin and sleep. Open Neuroendocrinol J. 3: 85–95.
12. Kopustinskiene DM, Bernatoniene J (2021) Molecular mechanisms of melatonin-mediated cell protection and signaling in health and disease. Pharmaceutics 13 (2):129.
13. Majidinia M, Reiter RJ, Shakouri SK, Yousefi B (2018) The role of melatonin, a multitasking molecule, in retarding the processes of ageing. Ageing Res. Rev. 47: 198–213.
14. Carrillo-Vico A, Guerrero JM, Lardone PJ, Reiter RJ (2005) A review of the multiple actions of melatonin on the immune system. Endocrine 27 (2): 189–200.
15. Carrillo-Vico A, Lardone PJ, Alvarez-Sanchez N, Rodriguez-Rodriguez, Guerrero J.M (2013) Melatonin: Buffering the immune system. Int. J. Mol. Sci. 14 (4): 8638–8683.
16. Acuna-Castroviejo D, et al. (2017) Melatonin, clock genes and mitochondria in sepsis. Cell. Mol. Life Sci. 74 (21): 3965–3987.
17. Won E, Na KS, Kim YK (2021) Associations between melatonin, neuroinflammation, and brain alterations in depression. Int. J. Mol. Sci. 23 (1): 305.
18. De la Fuente M, Miquel J (2009) An update of the oxidation-inflammation theory of aging: the involvement of the immune system in oxi-inflamm-aging. Curr. Pharm. Des. 15 (26): 3003–3026.
19. Hardeland R (2019) Aging, melatonin and the pro- and anti-inflammatory networks. Int. J. Mol. Sci. 20 (5):1223.
20. Gimenez VMM, et al. (2022) Melatonin as an anti-aging therapy for age-related cardiovascular and neurodegenerative diseases. Front Aging Neurosci. 14: 888292. doi: 10.3389/fnagi.2022.888292.
21. Farooq MA, et al. (2019) Acquiring control: The evolution of ROS-induced oxidative stress and redox signaling pathways in plant stress responses. Plant Physiol. Biochem. 141: 353-369.
22. Yang ZH, Wang J, Chan KS (2011) Spin accumulation in triplet Josephson junction. J Phys Condens Matter. 23 (8): 085701. doi: 10.1088/0953-8984/23/8/085701.
23. Gerschman R, Gilbert DL, Nye SW, Dwyer P, Fenn WO (1954) Oxygen poisoning and x-irradiation: a mechanism in common. Science 119 (3097): 623–626.
24. Watabe N, Ishida Y, Ochiai A, Tokuoka Y, Kawashima N (2007) Oxidation decomposition of unsaturated fatty acids by singlet oxygen in phospholipid bilayer membranes. J. Oleo Sci. 56 (2): 73–80.
25. Schieber M, Chandel NS (2014) ROS function in redox signaling and oxidative stress. Curr. Biol. 24 (10): R453-462.
26. Tan DX, et al. (2000) Significance of melatonin in antioxidative defense system: reactions and products. Biol. Signals Recept. 9 (3-4):137–159.
27. Cardoso S, Moreira PI (2022) Targeting mitochondria and redox dyshomeostasis in brain ageing: an update. In: Çakatay, U. (eds) Redox Signaling and Biomarkers in Ageing. Healthy Ageing and Longevity, vol 15. Springer, Cham. https://doi.org/10.1007/978-3-030-84965-8_8
28. Ursini F, Maiorino M, Forman HJ (2016) Redox homeostasis: The golden mean of healthy living. Redox Biol. 8: 205-215.
29. Ludovico P, Burhans WC (2014) Reactive oxygen species, ageing and the hormesis police. FEMS Yeast Res. 14 (1): 33-39.
30. Wang J, et al. (2019) Antioxidant and pro-oxidant activities of melatonin in the presence of copper and polyphenols in vitro and in vivo. Cells 8: 903.
31. He L, He T, Farrar S, Ji L, Liu T, Ma X (2017) Antioxidants maintain cellular redox homeostasis by elimination of reactive oxygen species. Cell Physiol. Biochem. 44(2):532-553. doi: 10.1159/000485089.
32. Okeke ES, Ogugofor MO, Nkwoemeka NE, Nweze EJ, Okoye CO (2022) Phytomelatonin: a potential phytotherapeutic intervention on COVID-19-exposed individuals. Microbes Infect. 24 (1): 104886.
33. Kuciel-Lewandowska J, et al. (2020) The impact of health resort treatment on the nonenzymatic endogenous antioxidant system. Oxid. Med. Cell Longev. 2020: 8423105.
34. Mannino G, Pernici C, Serio G, Gentile C, Bertea CM (2021) Melatonin and phytomelatonin: chemistry, biosynthesis, metabolism, distribution and bioactivity in plants and animals-an overview. Int. J. Mol. Sci. 22 (18): 9996.
35. Zhang H-M, Zhang Y (2014) Melatonin: a well-documented antioxidant with conditional pro-oxidant actions. J. Pineal Res. 57 (2):131–146.
36. Gurer-Orhan H, Suzen S (2015) Melatonin, its metabolites and its synthetic analogs as multi-faceted compounds: Antioxidant, prooxidant and inhibitor of bioactivation reactions. Curr. Med. Chem. 22 (4):490-499.
37. Karasek M (2004) Melatonin, human aging, and age-related diseases. Exp. Gerontol. 39 (11-12):1723–1729.
38. Finaud, J, Lac G, Filaire E (2012) Oxidative stress. Sports Medicine 36 (4): 327–358.
39. Suzen, S, Tucci P, Profumo E, Buttari B, Saso L (2022) A pivotal role of Nrf2 in neurodegenerative disorders: A new way for therapeutic strategies. Pharmaceuticals 15 (6): 692.
40. Sies H, Berndt C, Jones DP (2017) Oxidative stress. Annu. Rev. Biochem. 86: 715–748.
41. Sies, H, Jones D (2007) Editor-in-Chief: George Fink, Hardcover ISBN: 9780120885039, eBook ISBN: 9780080547961, Encyclopaedia of stress. 45–48
42. Ghezzi P (2014) Linkage of inflammation and oxidative stress via release of glutathionylated peroxiredoxin-2, which acts as a danger signal. Proc. Natl. Acad. Sci. 111 (33): 12157–12162.
43. Droge W (2002) Free radicals in the physiological control of cell function. Physiol. Rev. 82 (1): 47–95.
44. Birben E, Sahiner UM, Sackesen C, Erzurum S, Kalayci O (2012) Oxidative stress and antioxidant defense. World Allergy Organ. J. 5 (1): 9–19.
45. Matuszak Z, Reszka KJ, Chignell CF (1997) Reaction of melatonin and related indoles with hydroxyl radicals: EPR and spin trapping investigations. Free Radic. Biol. Med. 23 (3): 367–372.
46. Purushothaman A, Sheeja AA, Janardanan D (2020) Hydroxyl radical scavenging activity of melatonin and its related indolamines. Free Radic. Res. 54 (5): 373–383.
47. Reiter RJ, et al. (2003) Melatonin as an antioxidant: Biochemical mechanisms and pathophysiological implications in humans. Acta Biochim. Pol. 50 (4): 1129–1146.
48. Reiter RJ, Tan DX, Osuna C, Gitto E (2000) Actions of melatonin in the reduction of oxidative stress. A review. J. Biomed. Sci. 7 (6):444-458.
49. Vázquez J, et al. (2017) Melatonin reduces oxidative stress damage induced by hydrogen peroxide in saccharomyces cerevisiae. Front. Microbiol. 8:1066.
50. Liu F, Ng TB (2000) Effect of pineal indoles on activities of the antioxidant defense enzymes superoxide dismutase, catalase, and glutathione reductase, and levels of reduced and oxidized glutathione in rat tissues. Biochem. Cell Biol. 78 (4): 447–453.
51. Öztürk G, Coşkun S, Erbaş D, Hasanoǧlu E (2000) The effect of melatonin on liver superoxide dismutase activity, serum nitrate and thyroid hormone levels. Jap. J. Physiol. 50 (1): 149–153.
52. Tan DX, et al. (2005) Chemical and physical properties and potential mechanisms: melatonin as a broad spectrum antioxidant and free radical scavenger. Curr. Top. Med. Chem. 2 (2): 181–197.
53. Limón-Pacheco JH, Gonsebatt ME (2010) The glutathione system and its regulation by neurohormone melatonin in the central nervous system. Cent. Nerv. Syst. Agents Med. Chem. 10 (4): 287-297.
54. Montilla P, et al. (2001) Melatonin versus vitamin E as protective treatment against oxidative stress after extra-hepatic bile duct ligation in rats. J. Pineal Res. 31 (2): 138–144.
55. Galano A, Tan DX, Reiter RJ (2011) Melatonin as a natural ally against oxidative stress: a physicochemical examination. J. Pineal Res. 51 (1):1-16.
56. Borges LDS, et al. (2015) Melatonin decreases muscular oxidative stress and inflammation induced by strenuous exercise and stimulates growth factor synthesis. J. Pineal Res. 58 (2):166-172.
57. Gitto E, Aversa S, Reiter RJ, Barberi I, Pellegrino S (2011) Update on the use of melatonin in pediatrics. J. Pineal Res. 50 (1): 21-28.
58. Sanchez-Barcelo EJ, Mediavilla MD, Tan DX, Reiter RJ (2010) Clinical uses of melatonin: evaluation of human trials. Curr. Med. Chem. 17 (19): 2070-2095.
59. Bhattacharya P, Pandey AK, Paul S, Patnaik R (2014) Melatonin renders neuroprotection by protein kinase C mediated aquaporin-4 inhibition in animal model of focal cerebral ischemia. Life Sci. 100 (2): 97-109.
60. Paterniti I, Cordaro M, Esposito E, Cuzzocrea S (2016) The antioxidative property of melatonin against brain ischemia. Expert Rev. Neurother. 16 (7): 841-848.
61. Simko F, et al. (2014) Melatonin reduces cardiac remodeling and improves survival in rats with isoproterenol-induced heart failure. J. Pineal Res. 57 (2):177-184.
62. Jaworek J, Brzozowski T, Konturek SJ (2005) Melatonin as an organoprotector in the stomach and the pancreas. J. Pineal Res. 38 (2):73-83.
63. Sierra AF, Ramírez MLG, Campmany ACC, Martínez AR, Naveros BC (2013) In vivo and in vitro evaluation of the use of a newly developed melatonin loaded emulsion combined with UV filters as a protective agent against skin irradiation. J. Dermatol. Sci. 69 (3): 202-214.
64. Galano A, Reiter RJ (2018) Melatonin and its metabolites vs oxidative stress: From individual actions to collective protection. J. Pineal Res. 65 (1): e12514.
65. Pizza V, Agresta A, WD’Acunto C, Festa M, Capasso A (2012) Neuroinflamm-aging and neurodegenerative diseases: an overview. CNS Neurol. Disord. Drug Targets. 10 (5): 621–634.
66. Olanow CW (1993) A radical hypothesis for neurodegeneration. Trends Neurosci. 16 (11): 439–444.
67. Acuna-Castroviejo D, et. al. (2001) Melatonin, mitochondria, and cellular bioenergetics. J. Pineal Res. 30 (2): 65–74.
68. Madabhushi R, Pan L, Tsai LH (2014) DNA damage and its links to neurodegeneration. Neuron 83 (2): 266–282.
69. Kalliolia et al. (2014) Plasma melatonin is reduced in Huntington’s disease. Mov. Disord. 29 (12): 1511–1515.
70. Liu RY, Zhou JN, Van Heerikhuize J, Hofman MA, Swaab DF (1999) Decreased melatonin levels in postmortem cerebrospinal fluid in relation to aging, Alzheimer’s Disease, and apolipoprotein E-ε4/4 Genotype. J. Clin. Endocrinol. Metab. 84 (1): 323–327.
71. He R, et al. (2018) Melatonin resists oxidative stress-induced apoptosis in nucleus pulposus cells. Life Sci. 199: 122–130.
72. Lopez A, et al. (2009) Melatonin protects the mitochondria from oxidative damage reducing oxygen consumption, membrane potential, and superoxide anion production. J. Pineal Res. 46 (2): 188–198.
73. Carretero M, et al. (2009) Long-term melatonin administration protects brain mitochondria from aging. J. Pineal Res. 47 (2): 192–200.
74. Jauhari A, et al. (2020) Melatonin inhibits cytosolic mitochondrial DNA–induced neuroinflammatory signaling in accelerated aging and neurodegeneration. J. Clin. Invest. 130 (6): 3124–3136.
75. Rosales-Corral S, et al. (2003) Orally administered melatonin reduces oxidative stress and proinflammatory cytokines induced by amyloid-β peptide in rat brain: A comparative, in vivo study versus vitamin C and E. J. Pineal Res. 35 (2): 80–84.
76. Slominski AT, et al. (2017) Metabolism of melatonin in the skin: Why is it important? Exp. Dermatol. 26 (7): 563-568.
77. Slominski AT, et al. (2014) Local melatoninergic system as the protector of skin integrity. Int. J. Mol. Sci. 15: 1770519.
78. Bocheva G, et al (2022) Protective role of melatonin and its metabolites in skin aging. Int. J. Mol. Sci. 23 (3):1238-1252.
79. Ferlazzo N, et al. (2020) Is melatonin the cornucopia of the 21st century? Antioxidants (Basel). 9 (11):1088-102.
80. DeBalsi KL, Hoff KE, Copeland W.C (2017) Role of the mitochondrial DNA replication machinery in mitochondrial DNA mutagenesis, aging and age-related diseases. Ageing Res. Rev. 33: 89–104.
81. Birch-Machin MA., Bowman A (2016) Oxidative stress and ageing. Br. J. Dermatol. 175: 26–29.
82. Slominski AT, et al. (2018) Melatonin: a cutaneous perspective on its production, metabolism, and functions. J. Invest Dermatol. 138 (3): 490-499.
83. Rusanova I, et al. (2019) Protective effects of melatonin on the skin: future perspectives. Int. J. Mol. Sci. 20 (19): 4948-4962.
84. Kim TK, et al. (2013) Metabolism of melatonin and biological activity of intermediates of melatoninergic pathway in human skin cells. FASEB J. 27: 2742-2755.
85. Bilska B, et al. (2021) Mitochondrial function is controlled by melatonin and its metabolites in vitro in human melanoma cells. J. Pineal Res. 70 (3): e12728.
86. Kim TK, et al. (2015) Melatonin and its metabolites accumulate in the human epidermis in vivo and inhibit proliferation and tyrosinase activity in epidermal melanocytes in vitro. Mol. Cell Endocrinol. 404: 1- 8.
87. Kleszczyński K, et al. (2018) Melatonin and its metabolites ameliorate UVR-induced mitochondrial oxidative stress in human MNT-1 melanoma cells. Int. J. Mo.l Sci. 19 (12): e3786.
88. Kleszczyński K, et al. (2015) Melatonin compensates silencing of heat shock protein 70 and suppresses ultraviolet radiation-induced inflammation in human skin ex vivo and cultured keratinocytes. J. Pineal Res. 58 (1):117-126.
89. Tan DX, Reiter RJ (2019) Mitochondria: the birth place, battle ground and the site of melatonin metabolism in cells. Melatonin Res. 2 (1): 44-66.
90. Reiter RJ, et al. (2017) Melatonin as a mitochondria-targeted antioxidant: one of evolution's best ideas. Cell Mol. Life Sci. 74 (21): 3863-3881.
91. Kleszczyński K, et al. (2019) Melatonin exerts oncostatic capacity and decreases melanogenesis in human MNT-1 melanoma cells. J. Pineal Res. 67 (4): e12610.
92. Cabrera J, et al. (2010) Melatonin decreases cell proliferation and induces melanogenesis in human melanoma SK-MEL-1 cells. J. Pineal Res. 49 (1): 45- 54.
93. Slominski RM, et al. (2012) Melatonin membrane receptors in peripheral tissues: distribution and functions. Mol. Cell Endocrinol. 351:152– 166.
94. Bowman A, Birch-Machin MA (2015) Mitochondrial DNA as a biosensor of UV exposure in human skin. Methods Mol. Biol. 1265: 379– 388.
95. Kleszczyński K, Zillikens D, Fischer TW (2016) Melatonin enhances mitochondrial ATP synthesis, reduces reactive oxygen species formation, and mediates translocation of the nuclear erythroid 2-related factor 2 resulting in activation of phase-2 antioxidant enzymes (γ-GCS, HO-1, NQO1) in ultraviolet radiation-treated normal human epidermal keratinocytes (NHEK). J. Pineal Res. 61 (2):187-197.
96. Reiter RJ, Sharma R, Ma Q (2021) Switching diseased cells from cytosolic aerobic glycolysis to mitochondrial oxidative phosphorylation: A metabolic rhythm regulated by melatonin? J. Pineal Res. 70 (1): e12677.
97. Blask DE, et al. (2014) Light exposure at night disrupts host/cancer circadian regulatory dynamics: impact on the Warburg effect, lipid signaling and tumor growth prevention. PLoS One 9 (8): e102776.
98. Reiter RJ, et al. (2019) Inhibition of pyruvate dehydrogenase kinase: a proposed mechanism by which melatonin causes cancer cells to overcome cytosolic glycolysis, reduce tumor biomass and reverse insensitivity to chemotherapy. Melatonin Res. 2: 105- 119.
99. Zhao D, et al. (2019) Melatonin synthesis and function: evolutionary history in animals and plants. Front Endocrinol. (Lausanne) 10: 249-68.
100. Reiter RJ, et al. (2020) Melatonin inhibits Warburg-dependent cancer by redirecting glucose oxidation to the mitochondria: a mechanistic hypothesis. Cell Mol. Life Sci. 77 (13): 2527-2542.
101. Giudice A, et al. (2018) The effect of light exposure at night (LAN) on carcinogenesis via decreased nocturnal melatonin synthesis. Molecules 23 (6): 1308-1324.
102. Leon J, et al. (2004) Melatonin and mitochondrial function. Life Sci. 75 (7): 765–790.
103. Reiter RJ, et al. (2018) Melatonin mitigates mitochondrial meltdown: interactions with SIRT3. In.t J. Mol. Sci. 19: 8-12.
104. Acuña-Castroviejo D, et al. (2018) Melatonin actions in the heart; more than a hormone. Melatonin Res 1: 21–26.
105. Kim HS, et al. (2010) SIRT3 is a mitochondria-localized tumor suppressor required for maintenance of mitochondrial integrity and metabolism during stress. Cancer Cell 17 (1): 41–52.
106. Han L, et al. (2017) Melatonin protects against maternal obesity-associated oxidative stress and meiotic defects in oocytes via the SIRT3-SOD2-dependent pathway. J. Pineal Res. 63: 3-12.
107. Lv J, Liu F (2017) The role of serotonin beyond the central nervous system during embryogenesis. Front. Cell Neurosci. 11:74-88.
108. Slominski AT, et al. (2020) Characterization of serotonin and N-acetylserotonin systems in the human epidermis and skin cells. J. Pineal Res. 68 (2): e12626.
109. Reiter RJ, et al. (2022) Melatonin: highlighting its use as a potential treatment for SARS-CoV-2 infection. Cell Mol. Life Sci. 79 (3): 143.
110. Tian M, et al. (2021) HIF-1alpha promotes SARS-CoV-2infection and aggravates inflammatory responses to COVID-19. Signal Transduct. Target Ther. 6 (1): 308-318.
111. Florido J, et al. (2022) Understanding the mechanism of action of melatonin, which induces ROS production in cancer cells. Antioxidants (Basel). 11 (8):1621-1638.
112. Reiter RJ, Sharma R, Rosales-Corral S (2021) Anti-warburgeffect of melatonin: a proposed mechanism to explain its inhibition of multiple diseases. Int. J., Mol. Sci. 22 (2): 764-86.
113. Snider JM, et al. (2021) Group IIA secreted phospholipase A2 isassociated with the pathobiology leading to COVID-19 mortality. J. Clin. Invest. 131 (19): e149236.
114. Letsiou E, Htwe YM, Dudek SM (2021) Secretory phospholi-pase A2 enzymes in acute lung injury. Cell Biochem. Biophys. 79: 609–617.
115. Anderson G, Carbone A, Mazzoccoli G (2020) Aryl hydrocar-bon receptor role in co-ordinating SARS-CoV-2 entry and symptomatology: Linking cytotoxicity changes in COVID-19and cancers; modulation by racial discrimination stress. Biology (Basel). 9 (9): 249-258.
116. Karaaslan C, Suzen S (2015) Antioxidant properties of melatonin and its potential action in diseases. Curr. Top. Med. Chem. 15 (9): 894-903.
117. Garza-Lombó C, Pappa A, Panayiotidis MI, Franco R (2020) Redox homeostasis, oxidative stress and mitophagy. Mitochondrion. 51: 105-117.
118. Frank M, et al. (2012) Mitophagy is triggered by mild oxidative stress in a mitochondrial fission dependent manner. Biochim. Biophys. Acta 1823 (12): 2297-2310.
119. Atayik MC, Yanar K, Çakatay U (2022) Redox proteostasis in subcellular aging. In: Çakatay U (ed) Redox Signaling and Biomarkers in Ageing. Springer International Publishing Cham. pp 209–228.
120. Chen G, Kroemer G, Kepp O (2020) Mitophagy: an emerging role in aging and age-associated diseases. Front. Cell Dev. Biol. 8: 200.
121. Lin Q, et al. (2021) New insights into mitophagy and stem cells. Stem Cell Res. Ther. 12 (1): 452.
122. Atayik MC, Çakatay U. (2022) Mitochondria-targeted senotherapeutic interventions. Biogerontology. 23 (4):401-423.
123. Suofu Y, et al. (2017) Dual role of mitochondria in producing melatonin and driving GPCR signaling to block cytochrome c release. Proc. Natl. Acad. Sci. U .S .A. 114 (38): E7997–E8006.
124. Onphachanh X, et al. (2017) Enhancement of high glucose-induced PINK1 expression by melatonin stimulates neuronal cell survival: Involvement of MT(2) /Akt/NF-κB pathway. J. Pineal Res. 63 (2): e12427.
125. Atayik MC, Çakatay U. (2022) Melatonin-related signaling pathways and their regulatory effects in aging organisms. Biogerontology. 23 (5): 529-539. doi: 10.1007/s10522-022-09981-y.
126. Ding J, Sullivan D (2012) Aging and dry eye disease. Exp. Gerontol. 47 (7): 483-490.
127. Xu J, et al. (2022) Copolymer micelle-administered melatonin ameliorates hyperosmolarity-induced ocular surface damage through regulating PINK1-mediated mitophagy. Curr. Eye Res. 47 (5): 688-703.
128. Luo F, et al. (2020) Melatonin and autophagy in aging-related neurodegenerative diseases. Int. J. Mol. Sci. 21 (19): 7174.
129. Díaz-Casado ME, et al. (2016) Melatonin rescues zebrafish embryos from the parkinsonian phenotype restoring the parkin/PINK1/DJ-1/MUL1 network. J. Pineal Res. 61 (1): 96–107.
130. Bakula D, Scheibye-Knudsen M (2020) MitophAging: Mitophagy in aging and disease. Front. Cell Dev. Biol. 8: 239.
131. Hou Y, et al. (2019) Ageing as a risk factor for neurodegenerative disease. Nat. Rev. Neurol. 15 (10): 565–581.
132. Bubenik GA, Konturek SJ (2011) Melatonin and aging: prospects for human treatment. J. Physiol. Pharmacol. 62 (1):13-19.
133. Zhang J, et al. (2020) Synthesis of a new water-soluble melatonin derivative with low toxicity and a strong effect on sleep aid. ACS Omega 5 (12):6494-6499.
134. Alluri H, et al. (2016) Melatonin preserves blood-brain barrier integrity and permeability via matrix metalloproteinase-9 inhibition. PLoS One 11 (5): e0154427.
135. Galano A, Guzmán-López EG, Reiter RJ (2021) Potentiating the benefits of melatonin through chemical functionalization: possible impact on multifactorial neurodegenerative disorders. Int. J. Mol Sci. 22 (21):11584.
136. Tan DX, Hardeland R, Manchester LC, Galano A, Reiter RJ (2014) Cyclic-3-hydroxymelatonin (C3HOM), a potent antioxidant, scavenges free radicals and suppresses oxidative reactions. Curr. Med. Chem. 21 (13): 1557–1565.
137. Reiter RJ, Tan,DX, Galano A (2014) Melatonin reduces lipid peroxidation and membrane viscosity. Front. Physiol. 5: 377.
138. Burkhardt S, et al. (2002) DNA oxidatively damaged by chromium(III) and H2O2 is protected by the antioxidants melatonin, N1-acetyl-N2-formyl-5-methoxykynuramine, resveratrol and uric acid. Int. J. Biochem. Cell Biol. 33 (8): 775–783.
139. Maharaj DS, et al. (2005) 6-Hydroxymelatonin protects against quinolinic-acid-induced oxidative neurotoxicity in the rat hippocampus. J. Pharm. Pharmacol. 57 (7): 877–881.
140. Zhou H, et al. (2014) N-acetyl-serotonin offers neuroprotection through inhibiting mitochondrial death pathways and autophagic activation in experimental models of ischemic injury. J. Neurosci. 34 (8): 2967-2978.
141. Oxenkrug G, Requintina P, Bachurin S (2001) Antioxidant and antiaging activity of N-acetylserotonin and melatonin in the in vivo models. Ann. N. Y. Acad. Sci. 939: 190–199.
142. Jang SW, et al. (2010) N-acetylserotonin activates TrkB receptor in a circadian rhythm. Proc. Natl. Acad. Sci. U. S. A. 107 (8): 3876–3881.
143. Azouzi S, et al. (2017) Antioxidant and membrane binding properties of serotonin protect lipids from oxidation. Biophys. J. 112 (9): 1863-1873.
144. Reina M, et al. (2018) A computer-assisted systematic search for melatonin derivatives with high potential as antioxidants. Melatonin Res. 1 (1): 27-58.
145. Suzen S (2013) Melatonin and synthetic analogs as antioxidants. Curr. Drug Del. 10 (1): 71-75.
146. Galano A (2016) Computational-aided design of melatonin analogues with outstanding multifunctional antioxidant capacity. RSC Advances 6 (27): 22951-22963.
147. Ng TB, Liu F, Zhao L (2000) Antioxidative and free radical scavenging activities of pineal indoles. J. Neural. Transm. 107 (11): 1243–1251.
148. Suzen S, Bozkaya P, Coban T, Nebioglu D (2006) Investigation of the in vitro antioxidant behaviour of some 2-phenylindole derivatives: Discussion on possible antioxidant mechanisms and comparison with melatonin. J. Enzym. Inhib. Med. Chem. 21 (4): 405–411.
149. Ates-Alagöz Z, Coban T, Suzen S (2005) A comparative study: Evaluation of antioxidant activity of melatonin and some indole derivatives. Med. Chem. Res. 14: 169–179.
150. Shirinzadeh H, Eren B, Gurer-Orhan H Suzen, S, Özden S (2010) Novel indole-based analogs of melatonin: Synthesis and in vitro antioxidant activity studies. Molecules 15 (4): 2187–2202.
151. Yilmaz AD, Coban T, Suzen S (2012) Synthesis and antioxidant activity evaluations of melatonin-based analogue indole-hydrazide/hydrazone derivatives. J. Enzym. Inhib. Med. Chem. 27 (3):428–436.
152. Gurkok G, Coban T, Suzen S (2009) Melatonin analogue new indole hydrazide/hydrazone derivatives with antioxidant behavior: Synthesis and structureactivity relationships. J. Enzym. Inhib. Med. Chem. 24 (2): 506–515.
153. Suzen S, Cihaner SS, Coban T (2012) Synthesis and comparison of antioxidant properties of indole-based melatonin analogue indole amino acid derivatives. Chem. Biol. Drug Des. 79 (1): 76–83.
154. Reiter RJ, et al. (2015) Phytomelatonin: Assisting plants to survive and thrive. Molecules 20 (4): 7396-7437.
155. Reiter RJ, et al. (2008) Biogenic amines in the reduction of oxidative stress: Melatonin and its metabolites. Neuro. Endocrinol. Lett. 29 (4): 391-398.
156. Hardeland R (2014) Melatonin’s antioxidant properties: molecular mechanisms. In: Srinivasan V, Brzezinski A, Oter S, Chilcott SD, editors. Melatonin and Melatonergic Drugs in Clinical Practice. New Delhi: Springer India; 2014: 17–26. ISBN: 978-81-322-0825-9.
157. Dmitrzak-Weglarz M, Reszka E (2017) Pathophysiology of depression: molecular regulation of melatonin homeostasis - current status. Neuropsychobiology 76 (3): 117-129.
158. Prado NJ, Ferder L, Manucha W, Diez ER (2018) Anti-inflammatory effects of melatonin in obesity and hypertension. Curr. Hypertens Rep. 20 (5): 45.
159. Sarkar S, Chattopadhyay A, Bandyopadhyay, D (2021) Melatonin as a prospective metabolic regulator in pathologically altered cardiac energy homeostasis. Melatonin Res. 4 (2): 316-335.
160. Wan XD, et al. (2013) Long-term melatonin administration improves glucose homeostasis and insulin resistance state in high-fat-diet fed rats. Open. Life Sci. 8 (10): 958-967.
161. Owino S, Buonfiglio DDC, Tchio C, Tosini G (2019) Melatonin signaling a key regulator of glucose homeostasis and energy metabolism. Front. Endocrinol. (Lausanne). 10: 488.
162. Hong F, et al. (2020) Melatonin orchestrates lipid homeostasis through the hepatointestinal circadian clock and microbiota during constant light exposure. Cells 9 (2): E489.
163. Park WR, et al. (2022) Melatonin regulates iron homeostasis by inducing hepcidin expression in hepatocytes. Int. J. Mol. Sci. 23 (7): 3593.
164. Gonzalez A, Santofimia-Castaño P, Salido Gines M (2015) Melatonin, mitochondria, and Ca2+ homeostasis in the exocrine pancreas: an overview. Turk. J. Bio. 39: 801-812.
165. Jauhari A, et al. (2020) Melatonin inhibits cytosolic mitochondrial DNA-induced neuroinflammatory signaling in accelerated aging and neurodegeneration. J. Clin. Invest. 130 (6): 3124-3136. Erratum in: J Clin Invest. (2021) 131(9).
166. Yeung HM, Hung MW, Fung ML (2008) Melatonin ameliorates calcium homeostasis in myocardial and ischemia-reperfusion injury in chronically hypoxic rats. J. Pineal Res. 45 (4): 373-382.
167. Baburina Y, Lomovsky A, Krestinina O (2021) Melatonin as a potential multitherapeutic agent. J. Pers. Med. 11 (4): 274.
168. Dai CQ, Guo Y, Chu XY (2020) Neuropathic pain: the dysfunction of drp1, mitochondria, and ROS homeostasis. Neurotox. Res. 38 (3): 553-563.
169. Agil A, et al. (2021) Melatonin enhances the mitochondrial functionality of brown adipose tissue in obese-diabetic rats. Antioxidants (Basel) 10 (9): 482.
170. Paradies G, et al. (2010) Melatonin, cardiolipin and mitochondrial bioenergetics in health and disease. J. Pineal Res. 48 (4): 297-310.
171. Popov LD (2020) Mitochondrial biogenesis: An update. J. Cell Mol. Med. 24 (9): 4892-4899.

This work is licensed under a Creative Commons Attribution 4.0 International License.
For all articles published in Melatonin Res., copyright is retained by the authors. Articles are licensed under an open access Creative Commons CC BY 4.0 license, meaning that anyone may download and read the paper for free. In addition, the article may be reused and quoted provided that the original published version is cited. These conditions allow for maximum use and exposure of the work, while ensuring that the authors receive proper credit.
In exceptional circumstances articles may be licensed differently. If you have specific condition (such as one linked to funding) that does not allow this license, please mention this to the editorial office of the journal at submission. Exceptions will be granted at the discretion of the publisher.


