Estimated doses of melatonin for treating deadly virus infections: focus on COVID-19
Melatonin dose and viral infection
Abstract
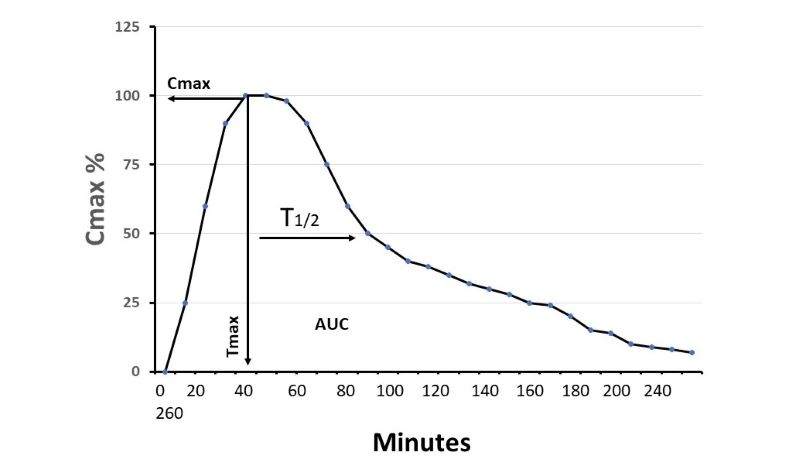
Increased evidence implies that melatonin may be a promising molecule for combating COVID-19 due to its potent antioxidative, anti-inflammatory and immunoregulatory capacities. A frequently asked question concerns the suitable dosage of melatonin for deadly virus infections including COVID-19 patients. The golden standards for a suitable dosage of medicine are safety and effectiveness. By reviewing the pharmacokinetics as well as animal studies and clinical trials of melatonin in the deadly viral infections and sepsis, we estimate that a dose of 8 mg/kg/day of melatonin is suitable for COVID-19 patients, especially for the severe cases. To maintain an elevated melatonin serum level lasting longer and smoother, this daily dose can be divided into 5 sub-doses with the initial dose of doubling over the other sub-doses. The recommended dose is in the ranges used to treat septic patients clinically and is devoid of any adverse effect; thus, it is safe. This dose is calculated from an effective dose which significantly reduces the mortality of virus-infected mice and is, therefore, assumed to be effective for COVID-19 severe patients. In our opinion, a dose or a medicine which can only improve the symptoms of mild or moderately severe patients of COVID-19 lack biological significance since virus infection is a self-limited disease and most of the patients with mild or moderate symptoms will recover by themselves whether treated or not. A meaningful treatment is to target the severe patients and significantly reduce the resulting mortality. The suggested melatonin dose is, thus, mainly recommended for the severe COVID-19 patients. The possibility of using suppositories for the delivery of highly dosed melatonin is also addressed, since long-term experience with this treatment is available for another disease.
References
2. Choy K-T, Wong AY-L, Kaewpreedee P, Sia SF, Chen D, Hui KPY, et al. (2020) Remdesivir, lopinavir, emetine, and homoharringtonine inhibit SARS-CoV-2 replication in vitro. Antiviral. Res. 178: 104786. doi:10.1016/j.antiviral.2020.104786.
3. Liu J, Cao R, Xu M, Wang X, Zhang H, Hu H, et al. (2020) Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. Cell Discov. 6: 16. doi:10.1038/s41421-020-0156-0.
4. Stower H. (2020) Lopinavir–ritonavir in severe COVID-19. Nat. Med. doi:10.1038/s41591-020-0849-9.
5. Ferner RE, Aronson JK (2020) Chloroquine and hydroxychloroquine in covid-19. BMJ 369: m1432. doi:10.1136/bmj.m1432.
6. Kujawski SA, Wong KK, Collins JP, Epstein L, Killerby ME, Midgley CM, et al. (2020) First 12 patients with coronavirus disease 2019 (COVID-19) in the United States. MedRxiv 2020: 2020.03.09.20032896. doi:10.1101/2020.03.09.20032896.
7. Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. (2020) First Case of 2019 Novel Coronavirus in the United States. N. Engl. J. Med. 382: 929–936. doi:10.1056/NEJMoa2001191.
8. Shie J-J, Fang J-M (2019) Development of effective anti-influenza drugs: congeners and conjugates – a review. J. Biomed. Sci. 26: 84. doi:10.1186/s12929-019-0567-0.
9. Amarelle L, Lecuona E, Sznajder JI (2017) Tratamiento antigripal: fármacos actualmente utilizados y nuevos agentes en desarrollo. Arch. Bronconeumol. 53: 19–26. doi:10.1016/j.arbres.2016.07.004.
10. Król E, Rychłowska M, Szewczyk B (2014) Antivirals--current trends in fighting influenza. Acta Biochim. Pol. 61:495–504.
11. Beigel J, Bray M (2008) Current and future antiviral therapy of severe seasonal and avian influenza. Antiviral Res. 78: 91–102. doi:10.1016/J.ANTIVIRAL.2008.01.003.
12. Li G, Fan Y, Lai Y, Han T, Li Z, Zhou P, et al. (2020) Coronavirus infections and immune responses. J. Med. Virol. 92: 424–32. doi:10.1002/jmv.25685.
13. Reiter RJ, Tan D-X, Rosales-Corral S, Galano A, Zhou X, Xu B. (2018) Mitochondria: Central Organelles for Melatonin′s Antioxidant and Anti-Aging Actions. Molecules 23: 509. doi:10.3390/molecules23020509.
14. Hardeland R (2019) Aging, melatonin, and the pro- and anti-inflammatory networks. Int. J. Mol. Sci. 20: 1223. doi:10.3390/ijms20051223.
15. Hardeland R (2018) Melatonin and inflammation-story of a double-edged blade. J. Pineal Res. 65: e12525. doi:10.1111/jpi.12525.
16. Luo J, Zhang Z, Sun H, Song J, Chen X, Huang J, et al. (2020) Effect of melatonin on T/B cell activation and immune regulation in pinealectomy mice. Life Sci. 242: 117191. doi:10.1016/j.lfs.2019.117191.
17. Tan DX, Hardeland R (2020) Potential utility of melatonin in deadly infectious diseases related to the overreaction of innate immune response and destructive inflammation: focus on COVID-19. Melatonin Res. 3: 120–43. doi:10.32794/mr11250052.
18. Zhou Y, Hou Y, Shen J, Huang Y, Martin W, Cheng F (2020) Network-based drug repurposing for novel coronavirus 2019-nCoV/SARS-CoV-2. Cell Discov. 6: 14. doi:10.1038/s41421-020-0153-3.
19. Zhang R, Wang X, Ni L, Di X, Ma B, Niu S, et al. (2020) COVID-19: Melatonin as a potential adjuvant treatment. Life Sci. 250:117583. doi:10.1016/j.lfs.2020.117583.
20. Shneider1 A, Kudriavtsev A, Vakhrusheva A (2020) Can melatonin reduce the severity of COVID-19 pandemic? Int. Rev. Immunol. doi:10.20944/PREPRINTS202004.0122.V1.
21. Tan D-X, Zheng X, Kong J, Manchester L, Hardeland R, Kim S, et al. (2014) fundamental issues related to the origin of melatonin and melatonin isomers during evolution: relation to their biological functions. Int. J. Mol. Sci. 15: 15858–15890. doi:10.3390/ijms150915858.
22. Tan D-X, Reiter RJ (2019) Mitochondria: the birth place, battle ground and the site of melatonin metabolism in cells. Melatonin Res. 2: 44–66. doi:10.32794/mr11250011.
23. Sugden D (1983) Psychopharmacological effects of melatonin in mouse and rat. J. Pharmacol. Exp. Ther. 227:587–591.
24. Barchas J, Dacosta F, Spector S (1967) Acute pharmacology of melatonin. Nature 214: 919–20. doi:10.1038/214919a0.
25. Jahnke G, Marr M, Myers C, Wilson R, Travlos G, Price C (1999) Maternal and developmental toxicity evaluation of melatonin administered orally to pregnant Sprague-Dawley rats. Toxicol. Sci. 50: 271–279. doi:10.1093/toxsci/50.2.271.
26. Nordlund JJ, Lerner AB (1977) The effects of oral melatonin on skin color and on the release of pituitary hormones. J. Clin. Endocrinol. Metab. 45: 768–774. doi:10.1210/jcem-45-4-768.
27. Voordouw BC, Euser R, Verdonk RE, Alberda BT, de Jong FH, Drogendijk AC, et al. (1992) Melatonin and melatonin-progestin combinations alter pituitary-ovarian function in women and can inhibit ovulation. J. Clin. Endocrinol. Metab. 74: 108–117. doi:10.1210/jcem.74.1.1727807.
28. Weishaupt JH, Bartels C, Pölking E, Dietrich J, Rohde G, Poeggeler B, et al. (2006) Reduced oxidative damage in ALS by high-dose enteral melatonin treatment. J. Pineal Res. 41: 313–323. doi:10.1111/j.1600-079X.2006.00377.x.
29. Nickkholgh A, Schneider H, Sobirey M, Venetz WP, Hinz U, Pelzl LH, et al. (2011) The use of high-dose melatonin in liver resection is safe: first clinical experience. J. Pineal Res. 50: 381–8. doi:10.1111/j.1600-079X.2011.00854.x.
30. Besag FMC, Vasey MJ, Lao KSJ, Wong ICK (2019) Adverse events associated with melatonin for the treatment of primary or secondary sleep disorders: a systematic review. CNS Drugs 33: 1167–186. doi:10.1007/s40263-019-00680-w.
31. Buscemi N, Vandermeer B, Hooton N, Pandya R, Tjosvold L, Hartling L, et al. (2006) Efficacy and safety of exogenous melatonin for secondary sleep disorders and sleep disorders accompanying sleep restriction: meta-analysis. BMJ 332: 385–393. doi:10.1136/bmj.38731.532766.F6.
32. Buscemi N, Vandermeer B, Hooton N, Pandya R, Tjosvold L, Hartling L, et al. (2005) The efficacy and safety of exogenous melatonin for primary sleep disorders. A meta-analysis. J. Gen. Intern. Med. 20: 1151–1158. doi:10.1111/j.1525-1497.2005.0243.x.
33. Foley HM, Steel AE (2019) Adverse events associated with oral administration of melatonin: A critical systematic review of clinical evidence. Complement. Ther. Med. 42: 65–81. doi:10.1016/j.ctim.2018.11.003.
34. Vural EMS, van Munster BC, de Rooij SE (2014) Optimal dosages for melatonin supplementation therapy in older adults: a systematic review of current literature. Drugs Aging 31: 441–451. doi:10.1007/s40266-014-0178-0.
35. Grilo-Bensusan I, Gómez-Delgado E, Gómez-Regife L (2015) Melatonin as a probable cause of diarrhoea. Rev. Esp. Enferm. Dig. 107: 119–120.
36. Bian Y, Lin C, Wang Z, Yang F (2020) Manic episode induced by melatonin: A case report. Bipolar Disord 22: 94–96. doi:10.1111/bdi.12869.
37. Brown GM, McIntyre RS, Rosenblat J, Hardeland R (2018) Depressive disorders: Processes leading to neurogeneration and potential novel treatments. Prog..Neuropsychopharmacol. Biol. Psychiatry 80: 189–204. doi:10.1016/j.pnpbp.2017.04.023.
38. Shimomura ET, Briones AJ, Gordon CJ, Warren WS, Jackson GF (2019) Case report of sudden death in a twin infant given melatonin supplementation: A challenging interpretation of postmortem toxicology. Forensic. Sci. Int. 304: 109962. doi:10.1016/j.forsciint.2019.109962.
39. Calvo JR, Guerrero JM, Osuna C, Molinero P, Carrillo-Vico A (2002) Melatonin triggers Crohn’s disease symptoms. J. Pineal Res. 32: 277–278. doi:10.1034/k.1600-079x.2002.01881.x.
40. Maldonado MD, Calvo JR (2008) Melatonin usage in ulcerative colitis: a case report. J. Pineal Res. 45: 339–340. doi:10.1111/j.1600-079X.2008.00584.x.
41. Chojnacki C, Wisniewska-Jarosinska M, Walecka-Kapica E, Klupinska G, Jaworek J, Chojnacki J (2011) Evaluation of melatonin effectiveness in the adjuvant treatment of ulcerative colitis. J. Physiol. Pharmacol. 62: 327–334.
42. Chojnacki C, Walecka-Kapica E, Lokieć K, Pawłowicz M, Winczyk K, Chojnacki J, et al. (2013) Influence of melatonin on symptoms of irritable bowel syndrome in postmenopausal women. Endokrynol. Pol. 64: 114–120.
43. Sulli A, Maestroni GJM, Villaggio B, Hertens E, Craviotto C, Pizzorni C, et al. (2002) Melatonin serum levels in rheumatoid arthritis. Ann. NY. Acad. Sci. 966: 276–283. doi:10.1111/j.1749-6632.2002.tb04227.x.
44. El-Awady HM, El-Wakkad ASE-D, Tawheed Saleh M, Ibraheem Muhammad S, Ghaniema EM (2007) Serum melatonin in juvenile rheumatoid arthritis: correlation with disease activity. Pakistan J. Biol. Sci. 10:1471–1476. doi:10.3923/pjbs.2007.1471.1476.
45. Tan D-X, Manchester LC, Terron MP, Flores LJ, Reiter RJ (2007) One molecule, many derivatives: A never-ending interaction of melatonin with reactive oxygen and nitrogen species? J. Pineal Res. 42: 28–42. doi:10.1111/j.1600-079X.2006.00407.x.
46. Hardeland R (2012) Melatonin in aging and disease -multiple consequences of reduced secretion, options and limits of treatment. Aging Dis. 3:194–225.
47. Forrest CM, Mackay GM, Stoy N, Stone TW, Darlington LG (2007) Inflammatory status and kynurenine metabolism in rheumatoid arthritis treated with melatonin. Br. J. Clin. Pharmacol. 64: 517–526. doi:10.1111/j.1365-2125.2007.02911.x.
48. Hong YG, Riegler JL (1997) Is melatonin associated with the development of autoimmune hepatitis? J. Clin. Gastroenterol. 25: 376–378. doi:10.1097/00004836-199707000-00020.
49. Gonciarz M, Mularczyk A, Szkudłapski D, J. Konturek S, Konturek PC (2019) A case of melatonin-induced biochemical flare in a patient with primary sclerosing cholangitis with features of autoimmune hepatitis. Gastroenterol. Rev. 14: 157–159. doi:10.5114/pg.2019.85901.
50. Fourman LT, Robert Meyer B (2013) Autoimmune hepatitis in association with ramelteon. J. Clin. Gastroenterol. 47: 651–654. doi:10.1097/MCG.0b013e31829174f0.
51. Carrillo-Vico A, Lardone P, Álvarez-Sánchez N, Rodríguez-Rodríguez A, Guerrero J (2013) Melatonin: buffering the immune system. Int. J. Mol. Sci.14: 8638–8683. doi:10.3390/ijms14048638.
52. Hardeland R, Cardinali DP, Brown GM, Pandi-Perumal SR (2015) Melatonin and brain inflammaging. Prog. Neurobiol. 127–128: 46–63. doi:10.1016/j.pneurobio.2015.02.001.
53. Hardeland R (2013) Melatonin and the theories of aging: a critical appraisal of melatonin’s role in antiaging mechanisms. J. Pineal Res. 55: 325–356. doi:10.1111/jpi.12090.
54. Floreani A, Restrepo-Jiménez P, Secchi MF, De Martin S, Leung PSC, Krawitt E, et al (2018) Etiopathogenesis of autoimmune hepatitis. J. Autoimmun. 95:133–143. doi:10.1016/J.JAUT.2018.10.020.
55. Rubio-Sastre P, Scheer FAJL, Gómez-Abellán P, Madrid JA, Garaulet M (2014) Acute melatonin administration in humans impairs glucose tolerance in both the morning and evening. Sleep 37: 1715–1719. doi:10.5665/sleep.4088.
56. Garaulet M, Gómez-Abellán P, Rubio-Sastre P, Madrid JA, Saxena R, Scheer FAJL (2015) Common type 2 diabetes risk variant in MTNR1B worsens the deleterious effect of melatonin on glucose tolerance in humans. Metabolism 64: 1650–1657. doi:10.1016/j.metabol.2015.08.003.
57. Hardeland R (2018) Recent findings in melatonin research and their relevance to the CNS. Cent. Nerv. Syst. Agents Med. Chem. 18: 102–114. doi:10.2174/1871524918666180531083944.
58. Lyssenko V, Nagorny CLF, Erdos MR, Wierup N, Jonsson A, Spégel P, et al. (2009) Common variant in MTNR1B associated with increased risk of type 2 diabetes and impaired early insulin secretion. Nat. Genet. 41: 82–88. doi:10.1038/ng.288.
59. Tuomi T, Nagorny CLF, Singh P, Bennet H, Yu Q, Alenkvist I, et al. (2016) Increased melatonin signaling is a risk factor for type 2 diabetes. Cell Metab. 23: 1067–1077. doi:10.1016/j.cmet.2016.04.009.
60. Moore DC, Paunier L, Sizonenko PC (1979). Effect of adrenergic stimulation and blockade on melatonin secretion in the human. Prog. Brain Res. 52: 517-521.
61. Brismar K, Mogensen L, Wetterberg L (1987) Depressed melatonin secretion in patients with nightmares due to β-adrenoceptor blocking drugs. Acta Med. Scand. 221: 155–158. doi:10.1111/j.0954-6820.1987.tb01260.x.
62. Brismar K, Hylander B, Eliasson K, Rössner S, Wetterberg L (1988) Melatonin secretion related to side-effects of β-blockers from the central nervous system. Acta Med. Scand. 223: 525–530. doi:10.1111/j.0954-6820.1988.tb17690.x.
63. McIntyre IM, Norman TR, Burrows GD, Armstrong SM (1993) Alterations to plasma melatonin and cortisol after evening alprazolam administration in humans. Chronobiol. Int. 10: 205–213. doi:10.3109/07420529309073889.
64. Hajak G, Rodenbeck A, Bandelow B, Friedrichs S, Huether G, Rüther E (1996) Nocturnal plasma melatonin levels after flunitrazepam administration in healthy subjects. Eur. Neuropsychopharmacol. 6: 149–153. doi:10.1016/0924-977x(96)00005-3.
65. Rosenstein RE, Chuluyan HE, Díaz MC, Cardinali DP (1990) GABA as a presumptive paracrine signal in the pineal gland. Evidence on an intrapineal GABAergic system. Brain Res. Bull. 25: 339–344. doi:10.1016/0361-9230(90)90080-J.
66. Michels KM, Morin LP, Moore RY (1990) GABAA/benzodiazepine receptor localization in the circadian timing system. Brain Res. 531: 16–24. doi:10.1016/0006-8993(90)90753-x.
67. Raskind MA, Burke BL, Crites NJ, Tapp AM, Rasmussen DD (2007) Olanzapine-induced weight gain and increased visceral adiposity is blocked by melatonin replacement therapy in rats. Neuropsychopharmacology 32: 284–288. doi:10.1038/sj.npp.1301093.
68. Rosenstein RE, Cardinali DP (1990) Central gabaergic mechanisms as targets for melatonin activity in brain. Neurochem. Int. 17: 373–379. doi:10.1016/0197-0186(90)90019-P.
69. Ursing C, Wikner J, Brismar K, Röjdmark S (2003) Caffeine raises the serum melatonin level in healthy subjects: An indication of melatonin metabolism by cytochrome P450(CYP)1A2. J. Endocrinol. Invest. 26: 403–406. doi:10.1007/BF03345194.
70. Shilo L, Sabbah H, Hadari R, Kovatz S, Weinberg U, Dolev S, et al. (2002) The effects of coffee consumption on sleep and melatonin secretion. Sleep Med. 3: 271–273. doi:10.1016/s1389-9457(02)00015-1.
71. MacKenzie T, Comi R, Sluss P, Keisari R, Manwar S, Kim J, et al. (2007) Metabolic and hormonal effects of caffeine: randomized, double-blind, placebo-controlled crossover trial. Metabolism 56: 1694–8. doi:10.1016/j.metabol.2007.07.013.
72. Bi X, Su Z, Yan H, Du J, Wang J, Chen L, Peng M, Chen S, Shen B, Li J (2020) Prediction of severe illness due to COVID-19 based on an analysis of initial fibrinogen to albumin ratio and platelet count. Platelets 5: 1-6. doi: 10.1080/09537104.2020.1760230.
73. Belen-Apak FB, Sarıalioğlu F (2020) Pulmonary intravascular coagulation in COVID-19: possible pathogenesis and recommendations on anticoagulant/thrombolytic therapy. J. Thromb. Thrombolysis doi: 10.1007/s11239-020-02129-0.
74. Tan DX, Korkmaz A, Reiter RJ, Manchester LC (2914) Ebola virus disease: potential use of melatonin as a treatment. J. Pineal Res. 57 (4): 381-384. doi: 10.1111/jpi.12186.
75. Nosjean O, Ferro M, Cogé F, Beauverger P, Henlin J-M, Lefoulon F, et al. (2000) Identification of the Melatonin-binding Site MT 3 as the Quinone Reductase 2. J. Biol. Chem. 275: 31311–31317. doi:10.1074/jbc.M005141200.
76. Fu Y, Buryanovskyy L, Zhang Z (2008) Quinone reductase 2 is a catechol quinone reductase. J. Biol. Chem. 283: 23829–35. doi:10.1074/jbc.M801371200.
77. Hardeland R. (2014) Agomelatine and the risk of hepatotoxicity. J. Symptoms Signs 3: 341–346.
78. Boutin JA (2016) Quinone reductase 2 as a promising target of melatonin therapeutic actions. Expert. Opin. Ther. Targets 20: 303–317. doi:10.1517/14728222.2016.1091882.
79. Paul P, Lahaye C, Delagrange P, Nicolas JP, Canet E, Boutin JA (1999) Characterization of 2-[125I]iodomelatonin binding sites in Syrian hamster peripheral organs. J. Pharmacol. Exp. Ther. 290: 334–340.
80. Ferry G, Hecht S, Berger S, Moulharat N, Coge F, Guillaumet G, et al. (2010) Old and new inhibitors of quinone reductase 2. Chem. Biol. Interact. 186: 103–109. doi:10.1016/j.cbi.2010.04.006.
81. Leung KKK, Shilton BH (2013) Chloroquine binding reveals flavin redox switch function of quinone reductase 2. J. Biol. Chem. 288: 11242–11251. doi:10.1074/jbc.M113.457002.
82. Pegan SD, Sturdy M, Ferry G, Delagrange P, Boutin JA, Mesecar AD (2011) X-ray structural studies of quinone reductase 2 nanomolar range inhibitors. Protein Sci. 20: 1182–1195. doi:10.1002/pro.647.
83. Mailliet F, Ferry G, Vella F, Berger S, Cogé F, Chomarat P, et al. (2005) Characterization of the melatoninergic MT3 binding site on the NRH:quinone oxidoreductase 2 enzyme. Biochem. Pharmacol. 71: 74–88. doi:10.1016/j.bcp.2005.09.030.
84. Calamini B, Santarsiero BD, Boutin JA, Mesecar AD (2008) Kinetic, thermodynamic and X-ray structural insights into the interaction of melatonin and analogues with quinone reductase 2. Biochem. J. 413: 81–91. doi:10.1042/BJ20071373.
85. Kwiek JJ, Haystead TAJ, Rudolph J (2004) Kinetic mechanism of quinone oxidoreductase 2 and its inhibition by the antimalarial quinolines. Biochemistry 43: 4538–4547. doi:10.1021/bi035923w.
86. Tan D-X, Manchester LC, Terron MP, Flores LJ, Tamura H, Reiter RJ (2007) Melatonin as a naturally occurring co-substrate of quinone reductase-2, the putative MT 3 melatonin membrane receptor: hypothesis and significance. J. Pineal Res. 43: 317–320. doi:10.1111/j.1600-079X.2007.00513.x.
87. Jin H, Zhang Z, Wang C, Tang Q, Wang J, Bai X, et al. (2018) Melatonin protects endothelial progenitor cells against AGE-induced apoptosis via autophagy flux stimulation and promotes wound healing in diabetic mice. Exp. Mol. Med. 50: 1–15. doi:10.1038/s12276-018-0177-z.
88. Fan T, Pi H, Li M, Ren Z, He Z, Zhu F, et al. (2018) Inhibiting MT2-TFE3-dependent autophagy enhances melatonin-induced apoptosis in tongue squamous cell carcinoma. J. Pineal Res. 64: e12457. doi:10.1111/jpi.12457.
89. Chen D, Li X, Liu X, Liu X, Jiang X, Du J, et al. (2017) NQO2 inhibition relieves reactive oxygen species effects on mouse oocyte meiotic maturation and embryo development†. Biol. Reprod. 97: 598–611. doi:10.1093/biolre/iox098.
90. Gould NL, Elkobi A, Edry E, Daume J, Rosenblum K (2020) Muscarinic-dependent miR-182 and QR2 expression regulation in the anterior insula enables novel taste learning. Eneuro. doi:10.1523/ENEURO.0067-20.2020.
91. Magagnoli J, Narendran S, Pereira F, Cummings T, Hardin JW, Sutton SS, et al. (2020) Outcomes of hydroxychloroquine usage in United States veterans hospitalized with Covid-19. MedRxiv doi:10.1101/2020.04.16.20065920.
92. Bauman JL, Tisdale JE (2020) Chloroquine and Hydroxychloroquine in the era of SARS - CoV2: caution on their cardiac toxicity. Pharmacotherapy doi:10.1002/phar.2387.
93. Mack HG, Kowalski T, Lucattini A, Symons RA, Wicks I, Hall AJ (2020) Genetic susceptibility to hydroxychloroquine retinal toxicity. Ophthalmic. Genet. 41: 159–170. doi:10.1080/13816810.2020.1747093.
94. Gautret P, Lagier J-C, Parola P, Hoang VT, Meddeb L, Sevestre J, et al. (2020) Clinical and microbiological effect of a combination of hydroxychloroquine and azithromycin in 80 COVID-19 patients with at least a six-day follow up: A pilot observational study. Travel. Med. Infect. Dis. 2020: 101663. doi:10.1016/j.tmaid.2020.101663.
95. Drugs.com: Usual adult dose for malaria prophylaxis. https://www.drugs.com/dosage/hydroxychloroquine.html#Usual_Adult_Dose_for_Malaria_Prophylaxis, accessed April 23, 2020
96. Meeran K, Jacobs MG (1993) Chloroquine poisoning. rapidly fatal without treatment. BMJ. 307: 49–50. doi:10.1136/bmj.307.6895.49.
97. Harpsøe NG, Andersen LPH, Gögenur I, Rosenberg J (2015) Clinical pharmacokinetics of melatonin: a systematic review. Eur. J. Clin. Pharmacol. 71: 901–909. doi:10.1007/s00228-015-1873-4.
98. Galley HF, Lowes DA, Allen L, Cameron G, Aucott LS, Webster NR (2014) Melatonin as a potential therapy for sepsis: a phase I dose escalation study and an ex vivo whole blood model under conditions of sepsis. J. Pineal Res. 56: 427–438. doi:10.1111/jpi.12134.
99. Andersen LPH, Werner MU, Rosenkilde MM, Harpsøe NG, Fuglsang H, Rosenberg J, et al. (2016) Pharmacokinetics of oral and intravenous melatonin in healthy volunteers. BMC. Pharmacol. Toxicol. 17: 8. doi:10.1186/s40360-016-0052-2.
100. Andersen LPH, Werner MU, Rosenkilde MM, Fenger AQ, Petersen MC, Rosenberg J, et al. (2016) Pharmacokinetics of high-dose intravenous melatonin in humans. J. Clin. Pharmacol. 56: 324–329. doi:10.1002/jcph.592.
101. Tan D, Manchester LC, Reiter RJ, Qi W, Hanes MA, Farley NJ (1999) High physiological levels of melatonin in the bile of mammals. Life Sci. 65: 2523–2529. doi:10.1016/s0024-3205(99)00519-6.
102. Carloni S, Proietti F, Rocchi M, Longini M, Marseglia L, D’Angelo G, et al. (2017) Melatonin pharmacokinetics following oral administration in preterm neonates. Molecules 22: 2115. doi:10.3390/molecules22122115.
103. Merchant NM, Azzopardi D V., Hawwa AF, McElnay JC, Middleton B, Arendt J, et al. (2013) Pharmacokinetics of melatonin in preterm infants. Br. J. Clin. Pharmacol. 76: 725–733. doi:10.1111/bcp.12092.
104. Huang S-H, Cao X-J, Liu W, Shi X-Y, Wei W (2010) Inhibitory effect of melatonin on lung oxidative stress induced by respiratory syncytial virus infection in mice. J. Pineal Res. 48: 109–116. doi:10.1111/j.1600-079X.2009.00733.x.
105. Valero N, Nery A, Bonilla E, Espina LM, Chacin-Bonilla L, Añez F, et al. (2009) Antagonistic effect of luzindole in mice treated with melatonin during the infection with the venezuelan equine encephalomyelitis virus. Neurochem. Res. 34: 268–273. doi:10.1007/s11064-008-9766-x.
106. Bonilla E, Valero-Fuenmayor N, Pons H, Chacin-Bonilla L (1997) Melatonin protects mice infected with Venezuelan equine encephalomyelitis virus. Cell Mol. Life Sci. 53: 430–434. doi:10.1007/s000180050051.
107. Montiel M, Bonilla E, Valero N, Mosquera J, Espina LM, Quiroz Y, et al. (2015) Melatonin decreases brain apoptosis, oxidative stress, and CD200 expression and increased survival rate in mice infected by Venezuelan equine encephalitis virus. Antivir. Chem. Chemother. 24: 99–108. doi:10.1177/2040206616660851.
108. Tuñón MJ, San Miguel B, Crespo I, Jorquera F, Santamaría E, Alvarez M, et al. (2011) Melatonin attenuates apoptotic liver damage in fulminant hepatic failure induced by the rabbit hemorrhagic disease virus. J. Pineal Res. 50: 38–45. doi:10.1111/j.1600-079X.2010.00807.x.
109. Crespo I, San-Miguel B, Sánchez DI, González-Fernández B, Álvarez M, González-Gallego J, et al. (2016) Melatonin inhibits the sphingosine kinase 1/sphingosine-1-phosphate signaling pathway in rabbits with fulminant hepatitis of viral origin. J. Pineal Res. 61: 168–176. doi:10.1111/jpi.12335.
110. Ben-Nathan D, Maestroni GJM, Lustig S, Conti A (1995) Protective effects of melatonin in mice infected with encephalitis viruses. Arch. Virol. 140: 223–230. doi:10.1007/BF01309858.
111. Huang S-H, Liao C-L, Chen S-J, Shi L-G, Lin L, Chen Y-W, et al. (2019) Melatonin possesses an anti-influenza potential through its immune modulatory effect. J. Funct. Foods 58: 189–198. doi:10.1016/J.JFF.2019.04.062.
112. Gitto E, Reiter RJ, Amodio A, Romeo C, Cuzzocrea E, Sabatino G, et al. (2004) Early indicators of chronic lung disease in preterm infants with respiratory distress syndrome and their inhibition by melatonin. J. Pineal Res. 36: 250–255. doi:10.1111/j.1600-079X.2004.00124.x.
113. Gitto E, Karbownik M, Reiter RJ, Tan DX, Cuzzocrea S, Chiurazzi P, et al. (2001) Effects of melatonin treatment in septic newborns. Pediatr. Res. 50: 756–760. doi:10.1203/00006450-200112000-00021.
114. Gitto E, Romeo C, Reiter R., Impellizzeri P, Pesce S, Basile M, et al. (2004) Melatonin reduces oxidative stress in surgical neonates. J. Pediatr. Surg. 39: 184–189. doi:10.1016/j.jpedsurg.2003.10.003.
115. Alamili M, Bendtzen K, Lykkesfeldt J, Rosenberg J, Gögenur I (2014) Melatonin suppresses markers of inflammation and oxidative damage in a human daytime endotoxemia model. J. Crit. Care 29: 184.e9-184.e13. doi:10.1016/j.jcrc.2013.09.006.
116. Alamili M, Bendtzen K, Lykkesfeldt J, Rosenberg J, Gögenur I (2014) Effect of melatonin on human nighttime endotoxaemia: randomized, double-blinded, cross-over study. In Vivo 28 (6): 1057-1063.
117. Henderson R, Kim S, Lee E (2018) Use of melatonin as adjunctive therapy in neonatal sepsis: A systematic review and meta-analysis. Complement. Ther. Med. 39: 131–136. doi:10.1016/j.ctim.2018.06.002.
118. El-Gendy FM, El-Hawy MA, Hassan MG (2018) Beneficial effect of melatonin in the treatment of neonatal sepsis. J. Matern. Fetal. Neonatal. Med. 31: 2299–2303. doi:10.1080/14767058.2017.1342794.
119. Tan DX, Xu B, Zhou X, Reiter RJ (2018) Pineal calcification, melatonin production, aging, associated health consequences and rejuvenation of the pineal gland. Molecules 23 (2): pii: E301. doi: 10.3390/molecules23020301.
120. Nair AB, Jacob S (2016) A simple practice guide for dose conversion between animals and human. J. Basic. Clin. Pharm. 7 (2): 27-31. doi: 10.4103/0976-0105.177703.
121. de Boer AG, Moolenaar F, de Leede LGJ, Breimer DD (1982) Rectal drug administration. Clin. Pharmacokinet. 7: 285–311. doi:10.2165/00003088-198207040-00002.
122. Ehrenreich H, Hardeland R, Nave K-H, Weishaupt J. (2008) Method of treating amyotrophic lateral sclerosis using melatonin. United States Patent no.: US 7,361,681 B2.

This work is licensed under a Creative Commons Attribution 4.0 International License.
For all articles published in Melatonin Res., copyright is retained by the authors. Articles are licensed under an open access Creative Commons CC BY 4.0 license, meaning that anyone may download and read the paper for free. In addition, the article may be reused and quoted provided that the original published version is cited. These conditions allow for maximum use and exposure of the work, while ensuring that the authors receive proper credit.
In exceptional circumstances articles may be licensed differently. If you have specific condition (such as one linked to funding) that does not allow this license, please mention this to the editorial office of the journal at submission. Exceptions will be granted at the discretion of the publisher.


