Pleiotropic roles of melatonin against oxidative stress mediated tissue injury in the gastrointestinal tract: An overview
Melatonin protects against oxidative stress-induced gastrointestinal damage
Abstract
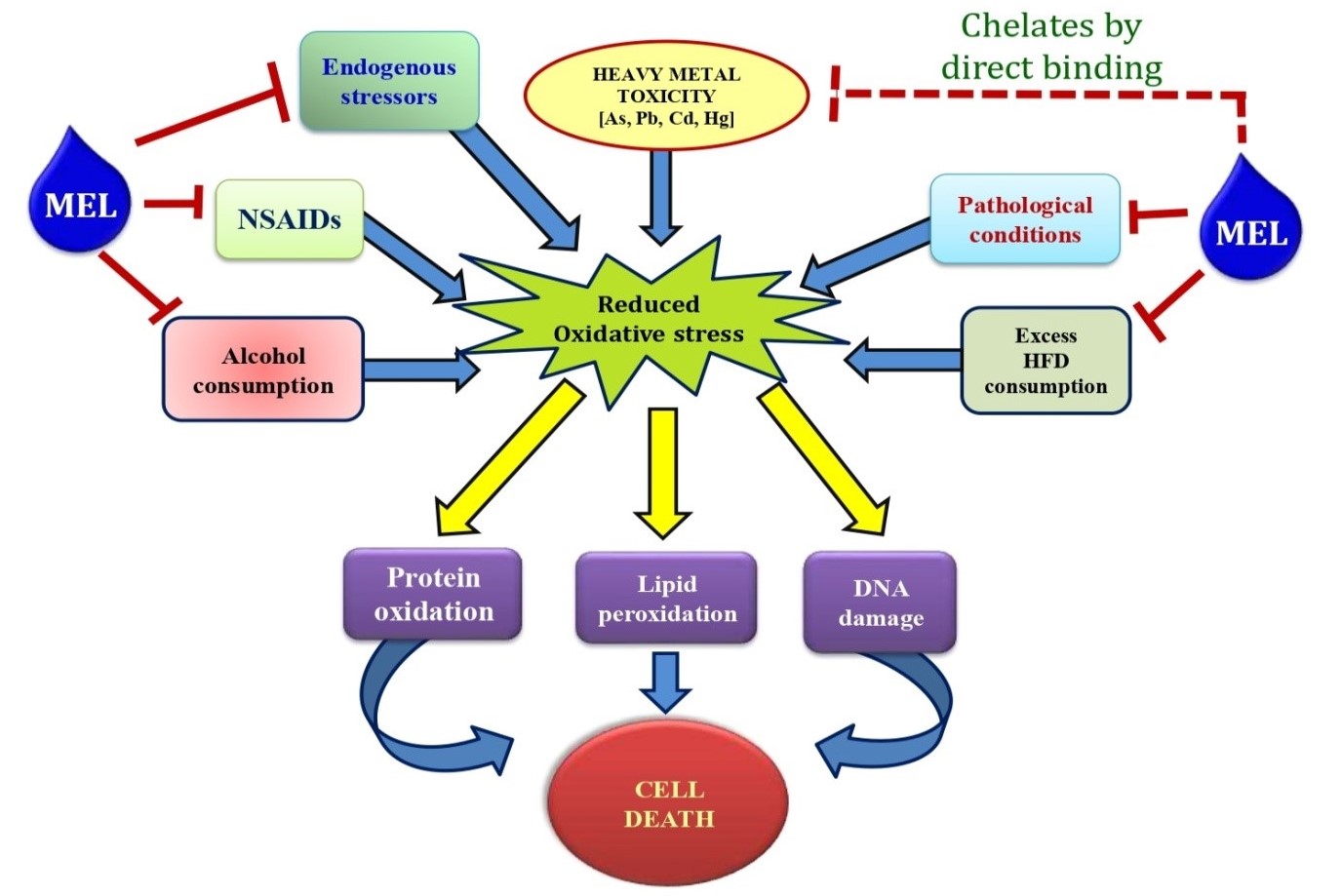
The excessive production of free radicals and/or reactive oxygen species (ROS) in gastrointestinal (GI) tract leads to oxidative damages in GI tissues with development of varied pathological conditions and clinical symptoms. Many endogenous as well as exogenous factors are involved in such pathogenesis, herein, focus was given to the factors of metal toxicity, non-steroidal anti-inflammatory drugs (NSAIDs), ischemia-reperfusion, consumption of high fat diet and alcohol, and different pathological conditions and diseases. Since ROS is more or less involved in the GI damages caused by these factors, therefore attempts have been made to develop appropriate therapeutic agents that possess antioxidant properties. Being a potent antioxidant and free radical scavenger, melatonin was suggested as a potent therapeutic answer to these GI damages. The discovery of different binding sites and receptors of melatonin in the GI tissues further proves its local actions to protect these tissues from oxidative stress. In the review, we attempt to try our best to summarize the current developments regarding the GI injuries caused by oxidative stress and the potential beneficial effects of melatonin on these injuries. The important molecular mechanisms associated with these changes were also highlighted in the discussion. We hope that this review will provide valuable information to consider melatonin as a suitable molecule used for GI tract protection.
References
2. Pal PK, Bhattacharjee B, Ghosh A, Chattopadhyay A, Bandyopadhyay D (2018) Adrenaline induced disruption of endogenous melatonergic system, antioxidant and inflammatory responses in the gastrointestinal tissues of male Wistar rat: an in vitro study. Melatonin Res. 1: 109–131. doi: 10.32794/mr11250007.
3. Pal PK, Bhattacharjee B, Chattopadhyay A, Bandyopadhyaya D (2019) Melatonin as an armament against non-steroidal anti-inflammatory drug (NSAID) induced gastric injury: An overview. Melatonin Res. 2: 116-138; doi: 10.32794/mr11250015.
4. Ghosh A, Bose G, Dey T, Pal PK, Mishra S, Ghosh AK, Chattopadhyay A, Bandyopadhyay D (2019) Melatonin protects against cardiac damage induced by a combination of high fat diet and isoproteronol exacerbated oxidative stress in male Wistar rat. Melatonin Res. 2: 9-31. DOI: 10.32794/mr11250009.
5. Bhattacharjee, B, Pal, PK, Ghosh, AK, Mishra A, Chattopadhyay A, Bandyopadhyay D (2019) Aqueous bark extract of Terminalia arjuna protects against cadmium-induced hepatic and cardiac injuries in male Wistar rats through antioxidative mechanisms. Food Chem. Toxicol. 124: 249–264. https://doi.org/10.1016/j.fct.2018.12.008.
6. Ryrfeldt A, Bannenberg G, Moldeus P (1993) Free radicals and lung disease. Br. Med. Bull. 49: 588–603.
7. Jackson MJ, O’Farrell S (1993) Free radicals and muscle damage. Br. Med. Bull.49: 630–641.
8. Pal PK, Hasan NK, Maitra SK (2016a) Gut melatonin response to microbial infection in carp Catla catla. Fish Physiol. Biochem. 42: 579–592. doi: 10.1007/s10695-015-0161-7.
9. Pal PK, Hasan NK and Maitra SK (2016b) Temporal relationship between the daily profiles of gut melatonin, oxidative status and major digestive enzymes in carp Catla catla. Biol. Rhythm Res. 47: 755–771. doi: 10.1080/09291016.2016.1191697.
10. Itoh M, Guth PH (1985) Role of oxygen-derived free radicals in hemorrhagic shock-induced gastric lesions in the rat. Gastroenterology 88: 1162–1167.
11. Bhattacharyya A, Chattopadhyay R, Mitra S, Crowe SE (2014) Oxidative stress: an essential factor in the pathogenesis of gastrointestinal mucosal diseases. Physiol. Rev. 94: 329–354. doi:10.1152/physrev.00040.2012.
12. Tay CH, Seah CS (1975) Arsenic poisoning from anti-asthmatic herbal preparations. Med. J. Aust. 2: 424-428.
13. Henning SJ, Leeper LL (1984) Duodenal uptake of lead by suckling and weanling rats. Bioi. Neonate 46: 27-35. doi: 10.1159/000242029.
14. Campbell JP, Alvares JA (1989) U.S. Public Health Service. Toxicological profile for arsenic.USEPA, Washington, DC. Acute arsenic intoxication. Am. Fam. Physician 40: 93-97.
15. Zalups RK (2000) Molecular interactions with mercury in the kidney. Pharmacol. Rev. 52: 113-143.
16. Koh DH, Bhatti P, Coble JB, Stewart PA, Lu W, Shu XO, Ji BT, Xue S, Locke SJ, Portengen L, Yang G, Chow WH, Gao YT, Rothman N, Vermeulen R, Friesen MC (2014) Calibrating a population-based job-exposure matrix using inspection measurements to estimate historical occupational exposure to lead for a population-based cohort in Shanghai, China. J. Exp. Sci. Env. Epid. 24: 9–16. doi: 10.1038/jes.2012.86.
17. Wongrakpanich S, Wongrakpanich A, Melhado K, Rangaswami J (2018) A comprehensive review of non-steroidal anti-inflammatory drug use in the elderly. Aging Dis. 9: 143-150. http://dx.doi.org/10.14336/AD.2017.0306.
18. Fritsche KL (2015) The science of fatty acids and inflammation. Adv. Nutr. 6: 293S–301S. doi: 10.3945/an.114.006940.
19. Beckman JS, Koppenol WH (1996) Nitric oxide, superoxide and peroxynitrite: the good, the bad and the ugly. Am. J. Physiol. 271: C1424–C1437. doi: 10.1152/ajpcell.1996. 271.5.c1424.
20. Victoni T, Coelho FR, Soares AL, de FA, Secher T, Guabiraba R, Erard F, de Oliveira-Filho RM, Vargaftig BB, Lauvaux G, Kama MA, Ryffe B, Moser R, Tavares-de-Lima W (2010) Local and remote tissue injury upon intestinal ischemia and reperfusion depends on the TLR/MyD88signalingpathway. Med. Microbiol. Immunol. 199: 35–42.
21. Tan DX, Chen LD, Poeggeler B, Manchester LC, Reiter RJ (1993) Melatonin: a potent, endogenous hydroxyl radical scavenger. Endocr. J. 1:57–60.
22. Kvetnoy IM, Ingel IE, Kvetnaia TV Malinovskaya NK, Rapoport SI, Raikhlin NT, Trofimov AV, Yuzhakov VV (2002) Gastrointestinal melatonin: cellular identification and biological role. Neuro. Endocrinol. Lett. 23:121–132.
23. Rakhlin NT, Kvetnoy IM, Tolkachev VN (1975) Melatonin may be synthesized in enterochromafinne cells. Nature 255: 344–345.
24. Bubenik GA (1999) Localization and physiological significance of gastrointestinal melatonin. In: R Watson (eds.) Melatonin in health promotion. CRC press, Boca Raton, Florida, pp. 21–39.
25. Dobocovich M, Mankowsha M (2005) Functional MP1 and MP2 melatonin receptors in mammals. Endocrine 27: 101–110. doi: 10.1385/ENDO:27:2:101.
26. Reiter RJ, Tan DX, Acuna-Castroviejo D, Burkhardt S, Karbownik M (2000) Melatonin: Mechanisms and actions as an antioxidant. Curr. Top. Biophys.24: 171–183.
27. Rodriguez C, Mayo JC, Sainz RM, Antolin I, Herrera F, Martin V, Reiter RJ (2004) Regulation of antioxidant enzymes: A significant role for melatonin. J. Pineal Res. 36: 1–9.
28. Ozdemir D, Uysal N, Tugyan K, Gonenc S, Acikgoz O, Aksu I, Ozkan H (2007) The effect of melatonin on endotoxemia-induced intestinal apoptosis and oxidative stress in infant rats. Intensive Care Med. 33: 511–516.
29. Trivedi PP, Jena GB (2013) Melatonin reduces ulcerative colitis-associated local and systemic damage in mice: investigation on possible mechanisms. Dig. Dis. Sci. 58: 3460–3474.
30. Khansari N, Shakiba Y, Mahmoudi M (2009) Chronic inflammation and oxidative stress as a major cause of age-related diseases and cancer. Recent Pat. Inflamm. Allergy Drug Discov. 3: 73–80. doi: 10.2174/187221309787158371.
31. Gavrilovic L-J, Stojiljkovic V, Kasapovic J, Pejic S, Todorovic A, Pajović B-S, Dronjak S (2012) Chronic physical stress changes gene expression of catecholamine biosynthetic enzymes in the adrenal medulla of adult rats. Acta Vet-Beograd. 62: 151–169. doi: 10.2478/acve-2014-0027.
32. Liu X, Wu W-K, Yu L, Sung J-J, Srivastava G, Zhang S-T, Cho C-H (2008) Epinephrine stimulates esophageal squamous-cell carcinoma cell proliferation via beta adrenoceptor-dependent transactivation of extracellular signal-regulated kinase/cyclooxygenase-2 pathway. J. Cell Biochem.105: 53–60. DOI: 10.1002/jcb.21802.
33. Yao H, Duan Z, Wang M, Awonuga A-O, Rappolee D, Xie Y (2009) Adrenaline induces chemoresistance in HT-29 colon adenocarcinoma cells. Cancer Genet. Cytogenet. 190: 81–87. doi: 10.1016/j.cancergencyto.2008.12.009.
34. Andrea Č, Lada Ž, Dijana Ž, Ninoslav D, Vladan B, DraganaD, Biljana SP (2014) Protective effect of dry olive leaf extract in adrenaline induced DNA damage evaluated using in vitro comet assay with human peripheral leukocytes. Toxicol. in Vitro 28: 451–456. doi: 10.1016/j.tiv.2013.12.014.
35. Rudra S, Mukherjee D, Dutta M, Ghosh A-K, Dey M, Basu A, Pattari S-K, Chattopadhyay A, Bandyopadhyay D (2014) Orally administered melatonin protects against adrenaline-induced oxidative stress in rat liver and heart: Involvement of antioxidant mechanism(s). J. Pharm. Res. 8: 303–320. http://jprsolutions.info/files/final-file-56bff9adee9ad8.28733292.pdf.
36. Raugstad T-S, Svanes K, Ulven A, Molster A (1979) Interaction between acute gastric ulcer and epinephrine-induced mucosal erosions in the rat: the significance of gastric acid secretion. Digestion 19: 70–72. doi: 10.1159/000198325.
37. Jaishankar M, Mathew BB, Shah MS, Gowda KRS (2014) Biosorption of Few Heavy Metal Ions Using Agricultural Wastes. J. Environ. Pollut. Human Health 2: 1–6. doi: 10.12691/jephh-2-1-1.
38. Wang G, Fowler BA (2008) Roles of biomarkers in evaluating interactions among mixtures of lead, cadmium and arsenic. Toxicol. Appl. Pharmacol. 233: 92–99. doi: 10.1016/j.taap.2008.01.017.
39. Morais S, Costa FG, Pereira ML (2012) Heavy metals and human health. In: Oosthuizen J, editor. Environmental health– emerging issues and practice. 10: 227–246. doi: 10.5772/29869.
40. Stohs SJ, Bagchi D (1995) Oxidative mechanisms in the toxicity of metalions. Free Radic. Biol. Med. 18: 321–336.
41. Flora SJS, Mittal M, Mehta A (2008) Heavy metal induced oxidative stress & its possible reversal by chelation therapy. Indian J. Med. Res. 128: 501–523.
42. Chen F, Ding M, Castranova V, Shi X (2001) Carcinogenic metals and NF-kB activation. Mol. Cell Biochem. 222: 159–171.
43. Richardson JB, Dancy BCR, Horton CL, Lee YS, Madejczyk MS, Xu ZZ, Ackermann G, Humphrey G, Palacios G, Knight R, Lewis JA (2018) Exposure to toxic metals triggers unique responses from the rat gut microbiota. Sci. Rep. 8: 6578. doi:10.1038/s41598-018-24931-w.
44. Evans CD, LaDow K, Schumann BL, Savage RE Jr, Caruso J, Vonderheide A, Succop P, Talaska G (2004) Effect of arsenic on benzo[a] pyrene DNA adduct levels in mouse skin and lung. Carcinogenesis 25: 493-497. doi: 10.1093/carcin/bgg199
45. Shi H, Shi X, Liu KJ (2004) Oxidative mechanism of arsenic toxicity and carcinogenesis. Mol. Cell Biochem. 255: 67-78.
46. Nava-Ruíz C, Méndez-Armenta M (2013) Cadmium, lead, thallium: occurrence, neurotoxicity and histopathological changes of the nervous system in Pollutant Diseases, Remediation and Recycling. vol. 4 of Environmental Chemistry for a Sustainable World, pp. 321–349.
47. ATSDR (1999) Toxicological Profile of Lead, US. Department of Health and Human Services Agency for Toxic Substances and Disease Registry, Washington, DC, USA.
48. Conrad ME, Barton JC (1978) Factors affecting the absorption and excretion of lead in the rat. Gastroenterol. 74: 731-740. doi: https://doi.org/10.1016/0016-5085(78)90253-6.
49. Valko M, Morris H, Cronin MTD (2005) Metals, toxicity and oxidative stress. Curr. Med. Chem. 12: 1161–1208. doi: 10.2174/0929867053764635.
50. Sugawara E, Nakamura K, Miyake T, Fukumura A, Seki Y (1991) Lipid peroxidation and concentration of glutathione in erythrocytes from workers exposed to lead. Br. J. Ind. Med. 48: 239–242.doi: 10.1136/oem.48.4.239.
51. Ahamed M, Verma S, Kumar A, Siddiqui M (2005) Environmental exposure to lead and its correlation with biochemical indices in children. Sci. Total Environ. 346: 48–55. doi: 10.1016/j.scitotenv.2004.12.019.
52. Yiin SJ, Lin TH (1995) Lead-catalyzed peroxidation of essential unsaturated fatty acid. Biol. Trace Elem. Res. 50: 167-172. doi: 10.1007/bf02789419.
53. IARC (1993) International Agency for research on Cancer, Beryllium, Cadmium. Mercury and exposures in the glass manufacturing industry, vol. 58, International Agency for Research on Cancer Monographs on the Evaluation of Carcinogenic Risks to Human (IARC), Lyon, France.
54. Shimada H, Yasutake A, Hirashima T, Takamure Y, Kitano T, Waalkes MP, Imamura Y (2008) Strain difference of cadmium accumulation by liver slices of inbred Wistar- Imamichi and Fischer 344 rats. Toxicol. in Vitro 22: 338–343. doi: 10.1016/j.tiv. 2007.09.013.
55. Wang Y, Fang J, Leonard SS, Rao KMK (2004) Cadmium inhibits the electron transfer chain and induces reactive oxygen species. Free Radic. Biol. Med. 36: 1434–1443. https://doi.org/10.1016/j.freeradbiomed.2004.03.010.
56. López E, Arce C, Oset-Gasque MJ, Ca˜nadas C, Gonz´alez MP (2006) Cadmium induces reactive oxygen species generation and lipid peroxidation in cortical neurons in culture. Free Radic. Biol. Med. 40: 940–951. https://doi.org/10.1016/j.freeradbiomed. 2005.10.062.
57. Kondoh M, Araragi S, Sato K, Higashimoto M, Takiguchi M, Sato M (2002) Cadmium induces apoptosis partly via caspase-9 activation in HL-60 cells. Toxicology 17: 111– 117.
58. Clifton II JC (2007) Mercury exposure and public health. Pediatr. Clin. Nor. Am. 54: 237–269. doi: 10.1016/j.pcl.2007.02.005.
59. Langford NJ, Ferner RE (1999) Toxicity of mercury. J. Hum. Hypertens. 13: 651–656. https://doi.org/10.1038/sj.jhh.1000896.
60. Hultberg B, Anderson A, Isaksson A (2001) Interaction of metals and thiols in cell damage and glutathione distribution: potentiation of mercury toxicity by dithiothreitol. Toxicol. 156: 93-100.
61. Barnes JL, McDowell EM, McNeil JS (1980) Studies on the pathophysiology of acute renal failure. V. Effect of chronic saline loading on the progression of proximal tubular injury and functional impairment following administration of mercuric chloride in the rat. Virchows Arch. B Cell Pathol. Incl. Mol. Pathol. 32: 233–260.
62. Siu SS, Yeung JH, Lau TK (2000) A study on placental transfer of diclofenac in first trimester of human pregnancy. Hum. Reprod. 15: 2423-2425. doi: 10.1093/humrep/15.11.2423
63. Kudo C, Kori M, Matsuzaki K, Yamai K, Nakajima A, Shibuya A, Niwa H, Kamisaki Y, Wada K (2003) Diclofenac inhibits proliferation and differentiation of neural stem cells. Biochem. Pharmacol. 66: 289-295. https://doi.org/10.1016/S0006-2952(03)00235-1.
64. Garner A (1992) Adaptation in the pharmaceutical industry, with particular reference to gastrointestinal damages and diseases. Scand. J. Gastroenterol. 27: 83-89.
65. Ragbetli MC, Ozyurt B, Aslan H, Odaci E, Gokcimen A, Sahin B, Kaplan S (2007) Effect of prenatal exposure to diclofenac sodium on Purkinje cell numbers in rat cerebellum: a stereological study. Brain Res. 1174: 130-135. doi: 10.1016/j.brainres. 2007.08.025.
66. Ennis ZN, Dideriksen D, Vaegter HB, Handberg G, Pottegard A (2016) Acetaminophen for chronic pain: a systematic review on efficacy. Basic Clin. Pharmacol. Toxicol. 118: 184-189. doi: 10.1111/bcpt.12527. doi: 10.1111/bcpt.12527.
67. Bjarnason I, Scarpignato C, Takeuchi K, Rainsford KD (2007) Determinants of the short-term gastric damage caused by NSAIDs in man. Aliment. Pharmacol. Ther. 26: 95–106. doi: 10.1111/j.1365-2036.2007.03348.x.
68. Awtry EH, Loscalzo J (2000) Cardiovascular drugs. aspirin. Circulation 101: 1206-1218.
69. García Rodríguez LA, Jick H (1994) Risk of upper gastrointestinal bleeding and perforation associated with individual non-steroidal anti-inflammatory drugs. Lancet 343: 769-772. https://doi.org/10.1016/S0140-6736(94)91843-0.
70. Yoshikawa T, Naito Y, Kishi A, Tomii T, Kaneko T, Jinuma S, Ichikawa H, Yasuda M, Takahashi S, Kondo M (1993) Role of active oxygen, lipid peroxidation, and antioxidants in the pathogenesis of gastric mucosal injury induced by indomethacin in rats. Gut 34: 732-737. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1374252.
71. Brzozowski T, Konturek PC, Konturek SJ, Pajdo R, Bielanski W, Brzozowska I, Stachura J, Han EG (1997) The role of melatonin and L-tryptophan in prevention of acute gastric lesions induced by stress, ethanol, ischemia, and aspirin. J. Pineal Res. 23: 79-89. https://doi.org/10.1111/j.1600-079X.1997.tb00339.x.
72. Banerjee RK (1990) Nonsteroidal anti-inflammatory drugs inhibit gastric peroxidase activity. Biochim. Biophys. Acta 1034: 275-280.
73. Das D, Bandyopadhyay D, Bhattacharjee M, Banerjee RK (1997) Hydroxyl radical is the major causative factor in stress-induced gastric ulceration. Free Radic. Biol. Med. 23: 8-18. https://doi.org/10.1016/S0891-5849(96)00547-3.
74. Naito Y, Yoshikawa T (2006) Oxidative stress Involvement and gene expression in indomethacin-induced gastropathy. Redox Rep. 11: 243–253. doi: 10.1179/135100006X 155021.
75. Chattopadhyay I, Bandyopadhyay U, Biswas K, Maity P, Banerjee RK (2006) Indomethacin inactivates gastric peroxidase to induce reactive-oxygen-mediated gastric mucosal injury and curcumin protects it by preventing peroxidise inactivation and scavenging reactive oxygen. Free Radic. Biol. Med. 40: 1397–1408. doi: 10.1016/ j.freeradbiomed.2005.12.016.
76. Mei Q, Diao L, Xu J, Liu X, Jin J (2011) A protective effect of melatonin on intestinal permeability is induced by diclofenac via regulation of mitochondrial function in mice. Acta Pharmacol. Sin. 32: 495–502. doi: 10.1038/aps.2010.225.
77. Phull PS, Green CJ, Jacyna MR (1995) A radical view of the stomach: the role of oxygen-derived free radicals and anti-oxidants in gastroduodenal disease. Eur. J. Gastroenterol. Hepatol. 7: 265–274.
78. Mallick IH, Yang W, Winslet MC, Seifalian AM (2004) Ischemia-reperfusion injury of the intestine and protective strategies against injury. Dig. Dis. Sci. 49: 1359–1377.
79. Benassi B, Fanciulli M, Fiorentino F, Porrello A, Chiorino G, Loda M, ZupiG,Biroccio A (2006) c-Mycphosphorylation is required for cellular response to oxidative stress. Mol. Cell 21: 509–519. doi: 10.1016/j.molcel.2006.01.009.
80. Sasaki M, Joh T (2007) Oxidative stress and ischemia-reperfusion injury in gastrointestinal tract and antioxidant, protective agents. J. Clin. Biochem. Nutr. 40: 1–12. doi: 10.3164/jcbn.40.1.
81. Heslin MJ, Hawkins A, Boedefeld W, Arnoletti JP, Frolov A, Soong R, Urist MM, Bland KI (2005) Tumor-associated down-regulation of 15-lipoxygenase-1 is reversed by celecoxib in colorectal cancer. Ann. Surg. 241: 941–946. doi: 10.1097/01.sla.0000164177.95620.c1.
82. Jarry A, Bach-Ngohou K, Masson D, Dejoie T, Lehur PA, Mosnier JF, Denis MG, Laboisse CL (2006) Human colonic myocytes are involved in post-ischemic inflammation through ADAM17-dependent TNF alpha production. Br. J. Pharmacol. 147: 64–72. doi: 10.1038/sj.bjp.0706449.
83. Nilsson UA, Lundgren O, Haglind E, Bylund-Fellenius AC (1989) Radical production during in vivo intestinal ischemia and reperfusion in the cat. Am. J. Physiol. 257: G409–G414.
84. Jaeschke H, Mitchell JR (1989) Mitochondria and xanthine oxidase both generate reactive oxygen species in isolated perfused rat liver after hypoxic injury. Biochem. Biophys. Res. Commun. 160: 140–147.
85. Zhang J, Piantadosi CA (1992) Mitochondrial oxidative stress after carbon monoxide hypoxia in the rat brain. J. Clin. Invest. 90: 1193–1199.
86. Bindoli A, Cavallini L, Rigobello MP, Coassin M, Di Lisa F (1988) Modification of the xanthine-converting enzymeof perfused rat heart during ischemia and oxidative stress. Free Radic. Biol. Med. 4: 163–167.
87. Liu JQ, Zelko IN, Folz RJ (2004) Reoxygenation-induced constriction in murine coronary arteries: the role of endothelial NADPH oxidase (gp91phox) and intra cellular superoxide. J. Biol. Chem. 279: 24493–24497.DOI: 10.1074/jbc.M402920200.
88. Grisham MB, Granger DN (1994) Metabolic sources of reactive oxygen metabolites during oxidant stress and ischemia with reperfusion. Clin. Chest Med. 10: 71–81.
89. Grace PA (1994) Ischaemia-reperfusion injury. Br. J. Surg. 81: 637–647.
90. Savini I, Catani MV, Evangelista D, Gasperi V, Avigliano L (2013) Obesity-associated oxidative stress: strategies finalized to improve redox state. Int. J. Mol. Sci. 21: 10497-538. doi: 10.3390/ijms140510497.
91. Auberval N, Dal S, Bietiger W, Pinget M, Jeandidier N, Maillard-Pedracini E, Valérie SK, Séverine S (2014) Metabolic and oxidative stress markers in wistar rats after 2 months on a high-fat diet. Diabetol. Metab. Syndr. 6: 130. doi: 10.1186/1758-5996-6-130.
92. Vargas-Robles H, Rios A, Arellano-Mendoza M, Escalante BA, Schnoor M (2015) Antioxidative diet supplementation reverses high-fat diet-induced increases of cardiovascular risk factors in mice. Oxid. Med. Cell Longev. 15: 1-9. doi: 10.1155/2015 /467471.
93. de La Serre CB, Ellis CL, Lee J, Ellis CL, Lee J, Hartman AL, Rutledge JC, Raybould HE (2010) Propensity to high-fat diet induced obesity in rats is associated with changes in the gut microbiota and gut inflammation. Am. J. Physiol. Gastrointest. Liver Physiol. 299: G440–G448. doi: 10.1152/ajpgi.00098.2010.
94. Kolios G, Valatas V, Ward SG (2004) Nitric oxide in inflammatory bowel disease: a universal messenger in an unsolved puzzle. Immunol. 113: 427–437. doi: 10.1111/j.1365 -2567.2004.01984.x.
95. Tan DX, Reiter RJ (2019) Mitochondria: the birth place, battle ground and the site of melatonin metabolism in cells. Melatonin Res. 2: 44-66. doi: https://doi.org/10.32794/ mr11250011.
96. Pessayre D, Mansouri A, Fromenty B (2002) Nonalcoholic steatosis and steatohepatitis. Mitochondrial dysfunction in steatohepatitis. Am. J. Physiol. Gastrointest. Liver Physiol. 282: G193-G199. doi: 10.1152/ajpgi.00426.2001.
97. Matsuzawa-Nagata N, Takamura T, Ando H, Nakamura S, Kurita S, Misu H, Ota T, Yokoyama M, Honda M, Miyamoto K, Kaneko S (2008) Increased oxidative stress precedes the onset of high-fat diet-induced insulin resistance and obesity. Metab. 57: 1071-1077. doi: 10.1016/j.metabol.2008.03.010.
98. McManus IR, Contag AO, Olson RE (1966) Studies on the identification and origin of ethanol in mammalian tissues. J. Biol. Chem. 241: 349–356.
99. Lester D, Keokosky WZ, Felzenberg F (1968) Effect of pyrazoles and other compounds on alcohol metabolism. Q. J. Stud. Alcohol 29: 449–454.
100. Schnabl B, Brenner DA (2014) Interactions between the intestinal microbiome and liver diseases. Gastroenterol. 146: 1513–1524. doi: 10.1053/j.gastro.2014.01.020.
101. Pronko P, Bardina L, Satanovskaya V, Kuzmich A, Zimatkin S (2002) Effect of chronic alcohol consumption on the ethanol-and acetaldehyde-metabolizing systems in the rat gastrointestinal tract. Alcohol Alcohol. 37: 229–235. https://doi.org/10.1093 /alcalc/37.3.229.
102. Vucevic D, Mladenovic D, Ninkovic M, Stankovic MN, Jorgacevic B, Stankovic MS, de Luka S, Radosavljevic T (2013). Influence of aging on ethanol-induced oxidative stress in digestive tract of rats. Hum. Exp. Toxicol. 32: 698. doi: 10.1177/0960327112467045.
103. Wild CP, Hardie LJ (2003) Reflux, Barrett’s oesophagus and adenocarcinoma: burning questions. Nat. Rev. Cancer 3: 676–684.
104. Song S, Guha S,Liu K, Buttar NS, Bresalier RS (2007) COX-2 induction by unconjugated bile acids involves reactive oxygen species-mediated signalling pathways in Barrett’s oesophagus and oesophageal adenocarcinoma. Gut 56: 1512–1521.doi: 10.1136/gut.2007.121244
105. Diakowska D, Krzystek KM, Lewandowski A, Grabowski K, Diakowski W (2008) Evaluation of 8-hydroxy deoxyguanosine, thiobarbituric acid-reactive substances and total antioxidant status as possible disease markers in oesophageal malignancies. Clin. Biochem. 41: 796–803. DOI: 10.1016/j.clinbiochem.2008.03.014.
106. O’Connor HJ, Schorah CJ, Habibzedah N, Axon AT, Cockel R (1989) Vitamin C in the human stomach: relation to gastric pH, gastroduodenal disease, and possible sources. Gut 30: 436–442.
107. Naito Y, Yoshikawa T, Ando T, Kishi A, Ueda S, Oyamada H, Kondo M (1992) Changes in superoxide dismutase activity in the gastric mucosa of peptic ulcer patients. J. Clin. Gastroenterol. 14: Suppl1: S131–S134.
108. Teshima S, Tsunawaki S, Rokutan K (1999) Helicobacter pylori lipopolysaccharide enhances the expression of NADPH oxidase components in cultured guinea pig gastric mucosal cells. FEBS Lett. 452: 243–246.
109. O’Hara AM, Bhattacharya A, Bai J, Mifflin RC, Smith MF Jr, Ryan KA, Scott KGE, Naganuma M, Casola A, Izumi T, Mitra S, Ernst PB, Crowe SE (2006) Interleukin-8 induction by Helicobacter pylori in human gastric epithelial cells is dependent on a purinic/ apyrimidinic endonuclease-1/redoxfactor-1. J. Immunol. 177: 7990–7999.
110. Ding SZ, Minohara Y, Fan XJ, Wang J, Reyes VE, Patel J, Kramer B, Boldogh I, Ernst PB, Crowe SE (2007) Helicobacter pylori infection induces oxidative stress and programmed cell death in human gastric epithelial cells. Infect. Immun. 75: 4030–4039. doi: 10.1128/IAI.00172-07.
111. Bhattacharya S, Mathew G, Jayne DG, Pelengaris S, Khan M (2009) 15-Lipoxygenase-1in colorectal cancer: a review. Tumour Biol. 30: 185–199. doi: 10.1159/000236864.
112. Davies GR, Simmonds NJ, Stevens TR, Grandison A, Blake DR, Rampton DS (1992) Mucosal reactive oxygen metabolite production in duodenal ulcer disease. Gut 33: 1467–1472. doi: 10.1136/gut.33.11.1467.
113. Jung HK, Lee KE, Chu SH, Yi SY (2001) Reactive oxygen species activity, mucosal lipoper-oxidation and glutathione in Helicobacter pylori-infected gastric mucosa. J. Gastroenterol. Hepatol. 16: 1336–1340.
114. O’Connor PM, Lapointe TK, Beck PL, Buret AG (2010) Mechanisms by which inflammation may increase intestinal cancer risk in inflammatory bowel disease. Inflamm. Bowel Dis. 16: 1411–1420. doi: 10.1002/ibd.21217.
115. Colgan SP, Taylor CT (2010) Hypoxia: anal arm signal during intestinal inflammation. Nat. Rev. Gastroenterol. Hepatol. 7: 281–287.doi: 10.1038/nrgastro.2010.39.
116. Iborra M, Moret I, Rausell F, Bastida G, Aguas M, Cerrillo E, Nos P, Beltran B (2011) Role of oxidative stress and antioxidant enzymes in Crohn’s disease. Biochem. Soc. Trans 39: 1102–1106. doi: 10.1042/BST0391102.
117. Kumar A, Wu H, Collier-Hyams LS, Hansen JM, Li T, Yamoah K, Pan ZQ, Jones DP, Neish AS (2007) Commensal bacteria modulate cullin-dependent signalling via generation of reactive oxygen species. EMBO J. 26: 4457–4466. doi: 10.1038/sj.emboj.7601867.
118. Sharma B, Singh S, Siddiqi NJ (2014) Biomedical implications of heavy metals induced imbalances in redox systems. Bio. Med. Res. Int. Article ID 640754, 26 pages.http://dx.doi.org/10.1155/2014/640754
119. Hooverand TD, Aposhian HV (1983) BAL increases the arsenic-74 content of rabbit brain. Toxicol. Appl. Pharm. 70: 160–162.
120. Risher JF, Amler SN (2005) Mercury exposure: evaluation and intervention. The inappropriate use of chelating agents in the diagnosis and treatment of putative mercury poisoning. Neuro. Toxicol. 26: 691–699.doi: 10.1016/j.neuro.2005.05.004.
121. ChisolmJr JJ, Thomas DJ (1985) Use of 2, 3-dimercaptopropane-1-sulfonatein treatment of lead poisoning in children. J. Pharmacol. Exp. Ther. 235: 665–669.
122. Zalups RK, Parks LD, Cannon VT, Barfuss DW (1998) Mechanisms of action of 2,3-dimercaptopropane-1-ulfonate and the transport, disposition, and toxicity of inorganic mer-curyinisolated perfused segments of rabbit proximal tubules. Molecul. Pharmacol. 54: 353–363.
123. Mayo JC, Tan DX, Sainz RM, Natarajan M, LopezBurillo S, Reiter RJ (2003) Protection against oxidative protein damage induced by metal catalyzed reaction or alkyl peroxyl radicals: comparative effects of melatonin and other antioxidants. Biochim. Biophys. Acta 1620: 139–150.
124. Bustamante J, Lodge JK, Marcocci L, Tritschler HJ, Packer L, Rihn BH (1998) Alpha-lipoic acid in liver metabolism and disease. Free Radic. Biol. Med. 24: 1023–1039.
125. Sumathi R, Baskaran G, Varalakshmi P (1996) Effect of DL-alpha-lipoic acid on tissue redox state in acute cadmium-challenged tissues. J. Nutr. Biochem. 7: 85–92.
126. Muller L (1989) Protective effects of DL-alpha-lipoicacid on cadmium induced deterioration of the rat’s patocytes. Toxicol. 58: 175–185.
127. Young IS, Woodside JV (2001) Antioxidants in health and disease. J. Clin. Pathol. 54: 176–186.
128. Rendon-Ramirez A, Cerbon-Solorzano J, Maldonado-Vega M, Quintanar-Escorza MA, Calderon-Salinas JV (2007) Vitamin-E reduces the oxidative damage on delta-aminolevulinic dehydratase induced by lead intoxication in rat erythrocytes. Toxicol. In Vitro 21: 1121–1126. doi: 10.1016/j.tiv.2007.04.019.
129. Tandon SK, Singh S, Dhawan M (1992) Preventive effect of vitaminE in cadmium intoxication. Biomed. Environ. Sci. 5: 39–45.
130. Quig D (1998) Cysteine metabolism and metal toxicity. Altern. Med. Rev.3: 262–270.
131. Shaikh ZA, Zaman K, Tang W, Vu T (1999) Treatment of chronic cadmium nephrotoxicity by N-acetylcysteine. Toxicol. Lett. 104: 137–142.
132. Santra A, Chowdhury A, Ghatak S, Biswas A, Dhali GK (2007) Arsenic induces apoptosis in mouse liver is mitochondria dependent and isabrogated by N-acetylcysteine. Toxicol. Applied Pharmacol. 220: 146–155.doi: 10.1016/j.taap.2006.12.029.
133. Mitra E, Ghosh AK, Ghosh D, Mukherjee D, Chattopadhyay A, Dutta S, Pattari S K and Bandyopadhyay D (2012) Protective effect of aqueous curry leaf (Murraya koenigii) extract against cadmium-induced oxidative stress in rat heart. Food Chem. Toxicol. 50: 1340–1353. doi: 10.1016/j.fct.2012.01.048.
134. Mitra E, Ghosh AK, Ghosh D, Firdaus SB, Mukherjee D, Chattopadhyay A, Pattari SK, Datta S, Bandyopadhyay D (2014) Ameliorative effect of aqueous tulsi leaf (Ocimum sanctum) extract against cadmium-induced oxidative stress in rat liver. Int. J. Pharm. Pharm. Sci. 5: 557-568.
135. Graham DY (1990) The relationship between nonsteroidal anti-inflammatory drug use and peptic ulcer disease. Gastroenterol. Clin. Nor. Am. 19: 171–182.
136. Wilhelmsen M, Amirian I, Reiter RJ, Rosenberg J, Gögenur I (2011) Analgesic effects of melatonin: A review of current evidence from experimental and clinical studies. J. Pineal Res. 51: 270–277. doi: 10.1111/j.1600-079x.2011.00895.x.
137. Lopez-Belmonte J, Whittle BJW, Moncada S (1993) The actions of nitric oxide donors in the prevention or induction of injury to the rat gastric mucosa. Br. J. Phamacol. 108: 73–78.
138. Reuter BK, Cirino G, Walkce JL (1994) Markedly reduced intestinal toxicity of a diclofenac derivative. Life Sci. 55: PL1-PL8. https://doi.org/10.1016/0024-3205 (94)90083-3.
139. Wallace JL (2006) Nitricoxide, aspirin-triggered lipoxins and NO-aspirinin gastric protection. Inflamm. Allergy Drug Targets 5: 133–137. doi: 10.2174/187152806776383116.
140. Soll AH, Weinstein WM, Kurata J, McCarthy D (1991) Nonsteroidal anti-inflammatory drugs and peptic ulcer disease. Ann. Intern. Med. 114: 387–319. doi: 10.18773/austprescr.2017.037.
141. Gavalas A, Hadjipetrou L, Kourounakis P (1998) Synthesis of novel derivatives of aroyl-aminoalcohols and 3-amino-substituted 1-phenylpropanols with potential anti-inflammatory and immunomodulating activity. J. Pharm. Pharmacol. 50: 583–591. https://doi.org/10.1111/j.2042-7158.1998.tb06891.x.
142. Farkouh ME, Kirshner H, Harrington RA, Ruland S, Verheugt FW, Schnitzer TJ, Burmester GR, Mysler E, Hochberg MC, Doherty M, Ehrsam E, Gitton X, Krammer G, Mellein B, Gimona A, Matchaba P, Hawkey CJ, Chesebro JH (2004) Comparison of lumiracoxib with naproxen and ibuprofen in the Therapeutic Arthritis Research and Gastrointestinal Event Trial (TARGET), cardiovascular outcomes: randomised controlled trial. Lancet 364: 675–684. doi: 10.1016/s0140-6736(04)16894-3.
143. Manchester LC, Coto-Montes A, Boga JA, Andersen LP, Zhou Z, Galano A, Vriend J, Tan DX, Reiter RJ (2015) Melatonin: an ancient molecule that makes oxygen metabolically tolerable. J. Pineal Res. 59: 403–419. doi: 10.1111/jpi.12267.
144. Reiter RJ, Mayo JC, Tan DX, Sainz RM, Alatorre-Jimenez M, Qin L (2016) Melatonin as an antioxidant: under promises but over delivers. J. Pineal Res. 61: 253–278. doi: 10.1111/jpi.12360.
145. Galano A, Tan DX, Reiter RJ (2018) Melatonin: a versatile protector against oxidative DNA damage. Molecules. 27: 23. doi: 10.3390/molecules23030530.
146. Konturek PC, Konturek SJ, Brzozowski T, Dembinski A, Zembala M, Mytar B, Hahn EG (1997) Gastroprotective activity of melatonin and its precursor, L-tryptophan, against stress-induced and ischemia-induced lesions is mediated by scavenge of oxygen radicals. Scand. J. Gastroenterol. 32: 433–438.
147. Martín M, Macías M, León J, Escames G, Khaldy H, Acuña- Castroviejo D (2002) Melatonin increases the activity of the oxidative phosphorylation enzymes and the production of ATP in rat brain and liver mitochondria. Int. J. Biochem. Cell. Biol. 34: 348–357.
148. Ercan F, Cetinel S, Contuk G, Cikler E, Sener G (2004) Role of melatonin in reducing water avoidance stress induced degeneration of the gastrointestinal mucosa. J. Pineal Res. 37: 113–121. doi: 10.1111/j.1600-079X.2004.00143.x.
149. Srinivasan V, Lauterbach EC, Ho KY, Acuña-Castroviejo D, Zakaria R, Brzezinski A (2012) Melatonin in antinociception: Its therapeutic applications. Curr. Neuropharmacol. 10: 167–178. doi: 10.2174/157015912800604489.
150. Becker-Andre M, Wiesenberg I, Schaeren-Wiemers N, Andre E, Missbach M, Saurat JH, Carlberg C (1994) Pineal gland hormone melatonin binds and activates an orphan of the nuclear receptor superfamily. J. Biol. Chem. 269: 28531–28534.
151. Witt-Enderby PA, Radio NM, Doctor JS, Davis VL (2006) Therapeutic treatments potentially mediated by melatonin receptors: potential clinical uses in the prevention of osteoporosis, cancer and as an adjuvant therapy. J. Pineal Res. 41: 297–305. doi: 10.1111/j.1600-079x.2006.00369.x.
152. Boutin JA, Audinot V, Ferry G, Delagrange P (2005) Molecular tools to study melatonin pathways and actions. Trends Pharmacol. Sci. 26: 412–419. doi:10.1016/j.tips. 2005.06.006.
153. Tan DX, Reiter RJ, Manchester LC, Yan MT, El-Sawi M, Sainz RM, Mayo JC, Kohen R, Allegra M, Hardeland R (2002) Chemical and physical properties and potential mechanisms: melatonin as a broad spectrum antioxidant and free radical scavenger. Curr. Top. Med. Chem. 2: 181-97. https://www.ncbi.nlm.nih.gov/pubmed/11899100.
154. Reiter RJ, Tan DX, Manchester LC, Qi W. (2001) Biochemical reactivity of melatonin with reactive oxygen and reactive nitrogen species: A review of the evidence. Cell. Biochem. Biophys. 34: 237–256. doi: 10.1385/CBB:34:2:237.
155. Cuzzocrea S, Reiter JR (2002) Pharmacological action of melatonin in acute and chronic inflammation. Curr. Top. Med. Chem. 2:153–165.
156. Nosál'ová V, Zeman M, Černá S, Navarová J, Zakálová M (2007) Protective effect of melatonin in acetic acid induced colitis in rats. J. Pineal Res. 42: 364–370. doi: 10.1111/j.1600-079X.2007.00428.x.
157. Torres-Farfan C, Richter HG, Rojas-García P, Vergara M, Forcelledo ML, Valladares LE, Torrealba F, Valenzuela GJ, Seron- Ferre M. (2003) mt1 Melatonin receptor in the primate adrenal gland: inhibition of adrenocorticotropin-stimulated cortisol production by melatonin. J. Clin. Endocrinol. Metab. 88: 450–458. doi: 10.1210/jc.2002-021048.
158. Saito S, Tachibana T, Choi YH, Denbow DM, Furuse M (2005) ICV melatonin reduces stress responses in neonatal chicks. Behav. Brain Res. 165: 197–203. doi: 10.1016/j.bbr.2005.06.045.
159. Lopez-Burillo S, Tan DX, Rodriguez-Gallego V, Manchester LC, Mayo JC, Sainz RM, Reiter RJ (2003) Melatonin and its derivatives cyclic 3-hydroxymelatonin, N1-acetyl-N2-formyl-5- methoxykynuramine, and 6-hydroxymelatonin reduced oxidative damage induced by Fenton reagents. J. Pineal Res. 34: 237–256. doi: 10.1034/j.1600-079x.2003.00025.x.
160. Poeggeler B, Reiter RJ, Hardeland R, Sewerynek E, Melchiorri D, Barlow-Walden LR (1995) Melatonin, a mediator of electron transfer and repair reactions acts synergistically with the chain breaking antioxidants ascorbate trolox and glutathione. Neuroendocrinol. Lett. 17: 87-92.
161. Raikhlin NT, Kvetnoy IM (1974) Lightening effect of the extract of human appendix mucosa on frog skin melanophores. Bull. Exp. Biol. Med. 8: 114–116.
162. Vakkuri O, Rintamaki H, Leppaluoto J (1985a) Presence of immunoreactive melatonin in different tissues of the pigeon. Gen. Comp. Endocrinol. 58: 69–75.
163. Vakkuri O, Rintamaki H, Leppaluoto J (1985b) Plasma and tissue concentrations of melatonin after midnight light exposure and pinealectomy in the pigeon. J. Endocrinol. 105: 263–268.
164. Huether G (1993) The contribution of extrapineal sites of melatonin synthesis to circulating melatonin levels in higher vertebrates. Experientia 49: 665–670.
165. Lee PPN, Shiu SYU, Chow PH, Pang SF (1995) Regional and diurnal studies on melatonin binding sites in the duck gastrointestinal tract. Biol. Signals 4: 212–224.
166. Menendez-Pelaez A, Buzzell GR (1992) Harderian gland indoles. In: Webb SM, Hoffman RA, Puig-Domingo ML, Reiter RJ (eds) Harderian glands: Porphyrin metabolism, behavioral, and endocrine effects. Springer, Berlin, pp. 219–234.
167. Chow PH, Lee PN, Poon AMS, Shiu SYW, Pang SF (1996) The gastrointestinal system: A site of melatonin paracrine action. In: Tang PL, Pang SF, Reiter RJ (eds.) Melatonin: A universal photoperiodic signal with diverse action. Front. Horm. Res. Basel, Karger, 21: 123–132.
168. Conti A, Conconi S, Hertens E, Skwarlo-Sonta K, Markowska M, Maestroni GJM (2000) Evidence of melatonin synthesis in mouse and human bone marrow. J. Pineal Res. 28: 193–202.
169. Fu Z, Kato H, Kotera N, Noguchi T, Sugahara K, Kubo T (2001) Regulation of hydroxyindole-O-methyltransferase gene expression in Japanese quail (Coturnixcoturnix japonica). Biosci. Biotechnol. Biochem. 65: 2504–2511. doi: 10.1271/bbb.65.2504.
170. Stefulj J, Hörtner M, Ghosh M, Schauenstein K, Rinner I, Wölfler A, Semmler J, Liebmann PM (2001) Gene expression of the key enzymes of melatonin synthesis in extrapineal tissues of the rat. J. Pineal Res. 30: 243–247.
171. Slominski A, Tobin DJ, Zmijewski MA, Wortsman J, Paus R (2008) Melatonin in the skin: synthesis, metabolism and functions. Trends Endocrinol. Metab.19: 17–24.
172. Hong GX, Pang SF (1995) N-Acetyltransferase activity in the quail (Cotornixcoturnixjap) duodenum. Comp. Biochem. Physiol. 112: 251–255.
173. Lovenberg W, Jequier E, Sjoerdsma A (1967) Tryptophan hydroxylation: Measurement in pineal gland, brain stem and carcinoid tumor. Science 155: 217–219.
174. Balemans MGM, Bary FAM, Legerstee WC, van Benthem J (1978) Estimation of the methylating capacity in the pineal gland of the rat with special reference to the methylation of N-acetylserotonin and 5-hydroxytryptophol separately. Experientia 34: 1434–1435.
175. Voisin P, Namboodiri MAA, Klein DC (1984) Arylamine N-acetyltransferase and arylalkylamine N-acetyltransferase in the mammalian pineal gland. J. Biol. Chem. 259: 10913–10918.
176. Axelrod J, Weissbach H. (1960) Enzymatic O-methylation of N-acetylserotonin to melatonin. Science 131: 1312–1312.
177. León J, Acuña-Castroviejo D, Escames G, Tan DX, Reiter RJ (2005) Melatonin mitigates mitochondrial malfunction. J. Pineal Res. 38: 1–9. doi: 10.1111/j.1600-079x.2004.00181.x.
178. Xu S, Pi H, Zhang L, Zhang N1, Li Y, Zhang H, Tang J, Li H, Feng M, Deng P, Guo P, Tian L, Xie J, He M, Lu Y, Zhong M, Zhang Y, Wang W, Reiter RJ, Yu Z, Zhou Z (2016) Melatonin prevents abnormal mitochondrial dynamics resulting from the neurotoxicity of cadmium by blocking calcium-dependent translocation of Drp1 to the mitochondria. J Pineal Res.60: 291-302. doi: 10.1111/jpi.12310.
179. Li M, Pi H, Yang Z, Reiter RJ, Xu S, Chen X, Chen C1, Zhang L, Yang M, Li Y, Guo P1, Li G, Tu M, Tian L, Xie J, He M, Lu Y, Zhong M, Zhang Y, Yu Z, Zhou Z (2016) Melatonin antagonizes cadmium-induced neurotoxicity by activating the transcription factor EB-dependent autophagy-lysosome machinery in mouse neuroblastoma cells. J. Pineal Res. 61: 353-69. doi: 10.1111/jpi.12353.
180. Sener G, Sehirli AO, Ayanoglu-Dülger G (2003) Melatonin protects against mercury (II)-induced oxidative tissue damage in rats. Pharmacol. Toxicol. 93: 290-296.
181. Zhang Y, Wei Z, Liu W, Wang J, He X, Huang H, Zhang J, Yang Z (2017) Melatonin protects against arsenic trioxide-induced liver injury by the upregulation of Nrf2 expression through the activation of PI3K/AKT pathway. Oncotarget. 8: 3773–3780. doi: 10.18632/oncotarget.13931.
182. Mishra S, Ghosh D, Dutta M, Chattopadhyay A, Bandyopadhyay D (2013) Melatonin protects against lead-induced oxidative stress in stomach,duodenum and spleen of male Wistar rats. J. Pharm. Res. 1: 997-1004.
183. Cabeza J, Alarcón-de-la-Lastra C, Jiménez D, Martín MJ, Motilva V (2003) Melatonin modulates the effects of gastric injury in rats: role of prostaglandins and nitric oxide. Neurosignals 12: 71–77.doi: 10.1159/000071816.
184. Ozturk H, Oztürk H, Yagmur Y, Uzunlar AK (2006) Effects of melatonin administration on intestinal adaptive response after massive bowel resection in rats. Dig. Dis. Sci. 51: 333–337. doi: 10.1007/s10620-006-3134-y.
185. Pandi-Perumal SR, Srinivasan V, Maestroni GJ, Cardinali DP, Poeggeler B, Hardeland R (2006) Melatonin: Nature's most versatile biological signal? FEBS J. 273: 2813–2838. doi: 10.1111/j.1742-4658.2006.05322.x.
186. Konturek PC, Konturek SJ, Burnat G, Brzozowski T, Brzozowska I, Reiter RJ (2008) Dynamic physiological and molecular changes in gastric ulcer healing achieved by melatonin and its precursor L-tryptophan in rats. J. Pineal Res. 45: 180–190. doi: 10.1111/j.1600-079x.2008.00574.x.
187. Hardeland R, Tan DX, Reiter RJ (2009) Kynuramines, metabolites of melatonin and other indoles: the resurrection of an almost forgotten class of biogenic amines. J. Pineal Res. 47: 109–124. doi: 10.1111/j.1600-079x.2009.00701.x.
188. Gitto E, Pellegrino S, Gitto P, Barberi I, Reiter RJ (2009) Oxidative stress of the newborn in the pre-and postnatal period and the clinical utility of melatonin. J. Pineal Res. 44: 128–139. doi: 10.1111/j.1600-079x.2008.00649.x.
189. Chen LJ, Gao YQ, Li XJ, Shen DH, Sun FY (2005) Melatonin protects against MPTP/MPP+ -induced mitochondrial DNA oxidative damage in vivo and in vitro. J. Pineal Res. 39: 34–42. doi: 10.1111/j.1600-079x.2005.00209.x.
190. Acuña-Castroviejo D, Escames G, León J, Carazo A, Khaldy H (2003) Mitochondrial regulation by melatonin and its metabolites. Adv. Exp. Med. Biol. 527: 549–557.
191. Hussein MR, Abu-Dief EE, Abd El-Reheem MH, Abd-Elrahman A (2005) Ultrastructural evaluation of the radioprotective effects of melatonin against X-ray-induced skin damage in Albino rats. Int. J. Exp. Pathol. 86: 45–55. doi: 10.1111/j.0959-9673.2005.00412.x.
192. Sener G, Sert G, Sehirli AO, Arbak S, Gedik N, Ayanoglu-Dülger G (2006) Melatonin protects against pressure ulcer-induced oxidative injury of the skin and remote organs in rats. J. Pineal Res. 40: 280–287. doi: 10.1111/j.1600-079x.2005.00313.x.
193. Jaworek J, Brzozowski T, Konturek SJ (2005) Melatonin as an organoprotector in the stomach and the pancreas. J. Pineal Res. 38: 73–83. doi: 10.1111/j.1600-079x.2004.00179.x.
194. Bandyopadhyay D, Ghosh G, Bandyopadhyay A, Reiter RJ (2004) Melatonin protects against piroxicam-induced gastric ulceration. J. Pineal Res. 36: 195–203. https://doi.org/10.1111/j.1600-079X.2004.00118.x.
195. Ates B, Yilmaz I, Geckil H, Iraz M, Birincioglu M, Fiskin K (2004) Protective role of melatonin given either before ischemia or prior to reperfusion on intestinal ischemia-reperfusion damage. J. Pineal Res. 37: 149–152.doi: 10.1111/j.1600-079X.2004.00148.x.
196. Kazez A, Demirbag M, Ustundag B, Ozercan IH, Saglam M (2000) The role of melatonin in prevention of intestinal ischemia-reperfusion injury in rats. J. Pediatr. Surg. 35: 1444–1448.
197. Ustundag B, Kazez A, Demirbag M, Canatan H, Halifeoglu I, and Ozercan IH (2000) Protective effect of melatonin on antioxidative system in experimental ischemia-reperfusion of rat small intestine. Cell Physiol. Biochem.10: 229–236. DOI: 10.1159/000016354.
198. Sileri P, Sica GS, Gentileschi P, Venza M, Benavoli D, Jarzembowski T, Manzelli A, Gaspari AL (2004) Melatonin reduces bacterial translocation after intestinal ischemia-reperfusion injury. Transplant Proc. 36: 2944–2946.doi: 10.1016/j.transproceed. 2004.10.085.
199. Ozacmak VH, Sayan H, Arslan SO, Altaner S, Aktas RG (2005) Protective effect of melatonin on contractile activity and oxidative injury induced by ischemia and reperfusion of rat ileum. Life Sci. 76: 1575–1588. doi: 10.1016/j.lfs.2004.08.031.
200. Ganguly K, Maity P, Reiter RJ, Swarnakar S (2005) Effect of melatonin on secreted and induced matrix metalloproteinase -9 and -2 activity during prevention of indomethacin-induced gastric ulcer. J. Pineal Res. 39: 307–315. doi: 10.1111/j.1600-079x.2005.00250.x.
201. Ganguly K, Kundu P, Banerjee A, Reiter RJ, Swarnakar S (2006) Hydrogen peroxide-mediated down regulation of matrixmetalloprotease-2 in indomethacin-induced acute gastric ulceration is blocked by melatonin and other antioxidants. Free Radic. Biol. Med. 41: 911–925. https://doi.org/10.1016/j.freeradbiomed.2006.04.022.
202. Brzozowska I, Konturek PC, Brzozowski T, Konturek SJ, Kwiecien S, Pajdo R, Drozdowicz D, Pawlik M, Ptak A, Hahn EG (2002) Role of prostaglandins, nitric oxide, sensory nerves and gastrin in acceleration of ulcer healing by melatonin and its precursor, L-tryptophan. J. Pineal Res. 32: 149–162. https://doi.org/10.1034/j.1600-079x.2002.1o811.x.
203. Brzozowski T, Konturek PC, ZwirskaKorczala K, Konturek SJ, Brzozowska I, Drozdowicz D, Sliwowski Z, Pawlik M, Pawlik WW, Hahn EG (2005) Importance of the pineal gland, endogenous prostaglandins and sensory nerves in the gastroprotective actions of central and peripheral melatonin against stress-induced damage. J. Pineal Res. 39: 375–385. https://doi.org/10.1111/j.1600-079X.2005.00264.x.
204. Carrillo-Vico A, Lardone PJ, Alvarez-Sánchez N, Rodríguez-Rodríguez A, Guerrero JM (2013) Melatonin: buffering the immune system. Int. J. Mol. Sci.14: 8638–8683. doi: 10.3390/ijms14048638.
205. Reiter RJ, Calvo JR, Karbownik M, Qi W, Tan DX (2000) Melatonin and its relation to the immune system and inflammation. Ann. N. Y. Acad. Sci. 917: 376–386. https://doi.org/10.1111/j.1749-6632.2000.tb05402.x.
206. Cuzzocrea S, Reiter RJ (2001) Pharmacological action of melatonin in shock, inflammation and ischemia/reperfusion injury. Eur. J. Pharmacol. 426: 1–10. https://doi.org/10.1016/S0014-2999(01)01175-X.
207. Lissoni P, Rovelli F, MeregalliS, Fumagalli L, Musco F, Brivio F, Brivio O, Esposti G (1997) Melatonin as a new possible anti-inflammatory agent. J. Biol. Regul. Homeost Agents 11: 157–159.
208. Agil A, Reiter RJ, Jiménez-Aranda A, Ibán-Arias R, Navarro-Alarcón M, Marchal JA, Adem A, Fernández-Vázquez G (2013) Melatonin ameliorates low-grade inflammation and oxidative stress in young Zucker diabetic fatty rats. J. Pineal R. 54: 381–388. doi: 10.1111/jpi.12012.
209. Mauriz JL, Collado PS, Veneroso C, Reiter RJ, González-Gallego J (2013) A review of the molecular aspects of melatonin’s anti-inflammatory actions: recent insights and new perspectives. J. Pineal Res. 54: 1–14.doi: 10.1111/j.1600-079X.2012.01014.x.
210. Dong Y, Fan C, Hu W, Jiang S, Ma Z, Yan X, Deng C, Di S, Xin Z, Wu G, Yang Y, Reiter RJ, Liang G (2016) Melatonin attenuated early brain injury induced by subarachnoid hemorrhage via regulating NLRP3 inflammasome and apoptosis signalling. J. Pineal Res. 60: 253–262.doi: 10.1111/jpi.12300.
211. Galano A, Tan DX, Reiter RJ (2011) Melatonin as a natural ally against oxidative stress: a physicochemical examination. J. Pineal Res. 51: 1–16. doi: 10.1111/j.1600-079X.2011.00916.x.
212. Baeuerle PA, Baltimore D (1996) NF-kappa B: ten years after. Cell 87: 13–20.
213. Li JH, Yu JP, Yu HG Xi-Ming Xu, Liang-Liang Yu, Jin Liu, He-Sheng Luo (2005) Melatonin reduces inflammatory injury through inhibiting NF-kappaB activation in rats with colitis. Mediators Inflamm. 2005: 185–193.doi: 10.1155/MI.2005.185.
214. Vriend J, Reiter RJ (2014) Melatonin as a proteasome inhibitor. Is there any clinical evidence? Life Sci. 115: 8–14.doi: 10.1016/j.lfs.2014.08.024.
215. Brzezinski A (1997) Melatonin in humans. N. Engl. J. Med. 336: 186–195. doi: 10.1056/NEJM199701163360306.
216. Volt H, García JA, Doerrier C, Díaz-Casado ME, Guerra-Librero A, López LC, Escames G, Tresguerres JA, Acuña-Castroviejo D (2016) Same molecule but different expression: aging and sepsis trigger NLRP3 inflammasome activation, a target of melatonin. J. Pineal Res. 60: 193–205.doi: 10.1111/jpi.12303.
217. D’emmanueleDi Villa Bianca R, Marzocco S, Di Paola R, Autore G, Pinto A, Cuzzocrea S, Sorrentino R (2004) Melatonin prevents lipopolysaccharide-induced hypore activity in rat. J. Pineal Res. 36: 146–154.
218. Deng WG, Tang ST, Tseng HP, Wu KK (2006) Melatonin suppresses macrophage cyclooxygenase-2 and inducible nitric oxide synthase expression by inhibiting p52 acetylation and binding. Blood 108: 518–524.doi: 10.1182/blood-2005-09-3691
219. Tamura EK, CeconE, Monteiro AW, Silva CL, Markus RP (2009) Melatonin inhibits LPS-induced NO production in rat endothelial cells. J. Pineal Res. 46: 268–274.doi: 10.1111/j.1600-079X.2008.00657.x.

This work is licensed under a Creative Commons Attribution 4.0 International License.
For all articles published in Melatonin Res., copyright is retained by the authors. Articles are licensed under an open access Creative Commons CC BY 4.0 license, meaning that anyone may download and read the paper for free. In addition, the article may be reused and quoted provided that the original published version is cited. These conditions allow for maximum use and exposure of the work, while ensuring that the authors receive proper credit.
In exceptional circumstances articles may be licensed differently. If you have specific condition (such as one linked to funding) that does not allow this license, please mention this to the editorial office of the journal at submission. Exceptions will be granted at the discretion of the publisher.


