Melatonin as an armament against non-steroidal anti-inflammatory drug induced gastric injury: An overview
Melatonin protects against NSAIDs
Abstract
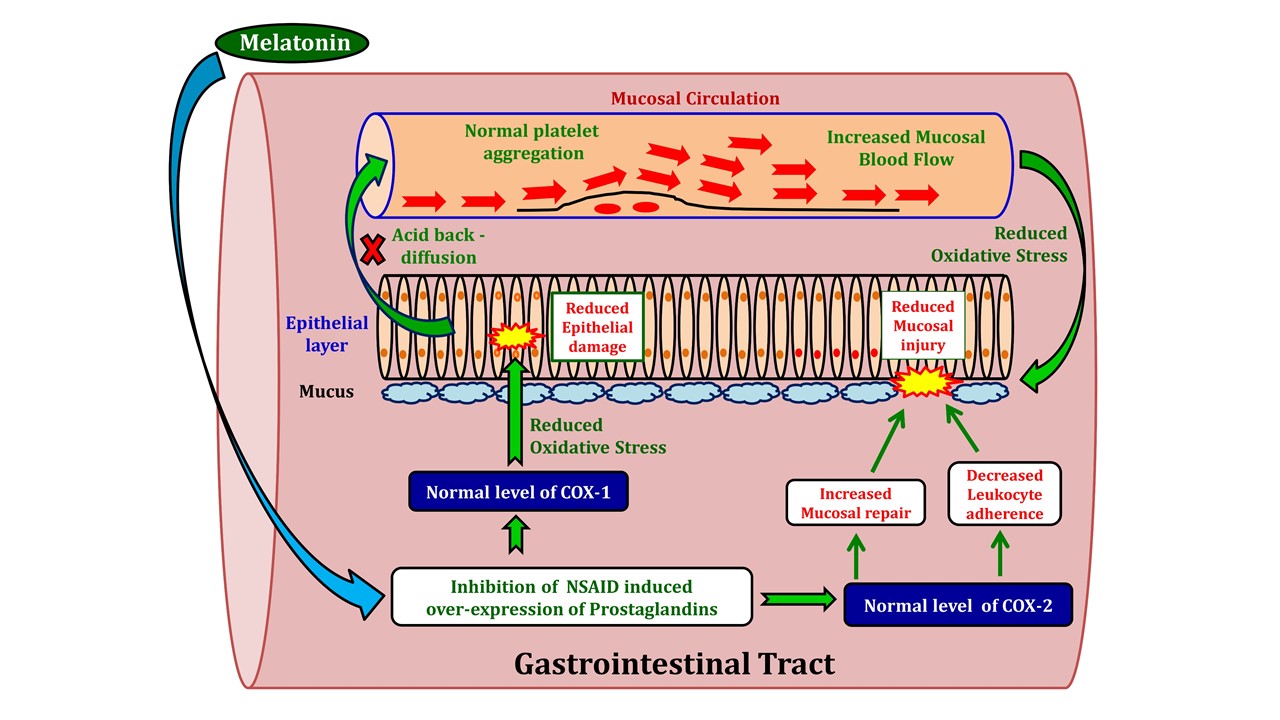
Non-steroidal anti-inflammatory drugs (NSAIDs) are the most widely prescribed medicines to treat numerous pathophysiological conditions clinically. However, growing evidence indicates the adverse effects of NSAIDs on the different vital organs, among which gastrointestinal (GI) tract seems to be the utmost target in most of the cases. NSAIDs promote over production of harmful reactive oxygen species (ROS) and reactive nitrogen species (RNS) in the gastric mucosa. These toxic species cause microvascular damage, increasing intestinal permeability, leading to the development of gastric lesions including ulcerations. Several strategies have been proposed to reduce the side effects of NSAIDs on the GI tissue, but most of them have failed to achieve this goal. Identification of an appropriate therapeutic strategy is urgently required. It is our opinion that this novel strategy to target GI damage induced by NSAID should include both anti-inflammatory and antioxidant properties. Under such a circumstance melatonin probably is the best choice for this purpose. Melatonin is a broad spectrum antioxidant and anti-inflammatory molecule. Numerous studies have reported the protective role of melatonin against gastric tissue damages caused by NSAIDs in animals or clinically. However, the underlying molecular mechanisms are not fully clarified. Thus, the present review attempts to gather the available information on this topic to provide a clear understanding on the exact scenario of this aspect.
References
2. Kudo C, Kori M, Matsuzaki K, Yamai K, Nakajima A, Shibuya A, Niwa H, Kamisaki Y, Wada K (2003) Diclofenac inhibits proliferation and differentiation of neural stem cells. Biochem.Pharmacol. 66: 289-295. https://doi.org/10.1016/S0006-2952(03)00235-1.
3. Wongrakpanich1 S, Wongrakpanich A, Melhado K, Rangaswami J (2018) A Comprehensive Review of Non-Steroidal Anti-Inflammatory Drug Use in The Elderly. Aging Dis. 9: 143-150. http://dx.doi.org/10.14336/AD.2017.0306
4. Ericson A, Källén BA (2001) Nonsteroidal anti-inflammatory drugs in early pregnancy. Reprod. Toxicol. 15: 371-375. DOI: 10.2174/138920012800166607.
5. Aygün D, Kaplan S, Odaci E, Mehmet EO,Muhammad EA (2012) Toxicity of non-steroidal anti-inflammatory drugs: a review of melatonin and diclofenac sodium association. Histol. Histopathol. 27: 417-436. DOI: 10.14670/HH-27.417.
6. Tenenbaum, J (1999) The epidemiology of non-steroidal anti-inflammatory drugs. Can. J. Gastroenterol. 13: 119–122.
7. Banerjee RK (1990) Nonsteroidal anti-inflammatory drugs inhibit gastric peroxidase activity. Biochim. Biophys. Acta. 1034: 275-280.
8. Wormsley KG (1988) Is Chronic Long-Term Inhibition of Gastric Secretion Really Dangerous? Scand. J. Gastroenterol. 146 (Suppl): 166-174.
9. Lambersts R, Crentzfeldt W, Struber HG (1993) Long-term omeprazole therapy in peptic ulcer disease: gastrin, endocrine cell growth, and gastritis. Life Sci. 60: 169-174.
10. Koelz HR (1986) Scand. J. Gastroenterol. 21: 156-164.
11. Wormsley KG (1984) Assessing the safety of drugs for the long-term treatment of peptic ulcers. Gut 25: 1416-1423.
12. Hansten PD (1994) In: A Pharmacologic Approach to Gastrointestinal Disorders, Lewis, J.H., Ed., Academic Press, New York, pp. 535-540.
13. Kourounakis PN, Tsiakitzis K, Kourounakis AP, Galanakis D (2000) Reduction of gastrointestinal toxicity of NSAIDs via molecular modifications leading to antioxidant anti-inflammatory drugs. Toxicol. 144: 205–210. https://doi.org/10.1016/S0300-483X(99)00208-5.
14. Bandyopadhyay D, Biswas K, Bhattacharyya M, Reiter RJ, Banerjee RK (2001) Gastric toxicity and mucosal ulceration induced by oxygen derived reactive species: protection by melatonin. Curr. Mol. Med. 1: 501-513.DOI: 10.2174/1566524013363483.
15. Bhattacharyya A, Chattopadhyay R, Mitra S, Crowe SE (2014) Oxidative stress: an essential factor in the pathogenesis of gastrointestinal mucosal diseases. Physiol. Rev. 94: 329–354. DOI: 10.1152/physrev.00040.2012.
16. Hassan A, Martin E, Puig-Parellada P (1998) Role of antioxidants in gastric mucosal damage induced by indomethacin in rats. Methods Find. Exp. Clin. Pharmacol. 20: 849–854. DOI: 10.1358/mf.1998.20.10.487540.
17. Chattopadhyay I, Bandyopadhyay U, Biswas K, Maity P, Banerjee RK (2006) Indomethacin inactivates gastric peroxidase to induce reactive-oxygen-mediated gastric mucosal injury and curcumin protects it by preventing peroxidise inactivation and scavenging reactive oxygen. Free Radic. Biol. Med. 40: 1397–1408. DOI: 10.1016/j.freeradbiomed.2005.12.016.
18. Slomiany BL, Slomiany A (2000) Role of endothelin-converting enzyme-1 in the suppression of constitutive nitric oxide synthase in rat gastric mucosal injury by indomethacin. Scand. J. Gastroenterol. 35: 1131–1136.
19. Naito Y, Yoshikawa T (2006) Oxidative stress Involvement and gene expression in indomethacin-induced gastropathy. Redox Rep. 11: 243–253. DOI: 10.1179/135100006X155021.
20. Kotler M, Rodriguez C, Sáinz RM, Antolín I, and Menédez-Peláez A (1998) Melatonin increases gene expression for antioxidant enzymes in rat brain cortex. J. Pineal Res. 24: 83–89. https://doi.org/10.1111/j.1600-079X.1998.tb00371.x.
21. Lerner AB, Case JD, Lee TH, Mori W (1958) Isolation of melatonin, the pineal factor that lightens melanocytes. J. Am. Chem. Soc. 80: 2587–2587.
22. Tan DX, Chen LD, Poeggeler B, Manchester LC, Reiter RJ (1993) Melatonin: a potent, endogenous hydroxyl radical scavenger. Endocr. J. 1: 57–60.
23. Rodriguez C, Mayo JC, Sainz RM, Antolin I, Herrera F, Martin V, Reiter RJ (2004) Regulation of antioxidant enzymes: A significant role for melatonin. J. Pineal Res. 36: 1–9. https://doi.org/10.1046/j.1600-079X.2003.00092.x.
24. Jan JE, Hamilton D, Seward N, Fast DK, Freeman RD, Laudon, M (2000) Clinical trials of controlled-release melatonin in children with sleep–wake cycle disorders. J. Pineal Res. 29: 34-39. https://doi.org/10.1034/j.1600-079X.2000.290105.x.
25. Bandyopadhyay D, Biswas K, Bandyopadhyay U, Banerjee, RK (2000) Melatonin protects against stress-induced gastric lesions by scavenging the hydroxyl radical. J. Pineal Res. 29: 143–151. https://doi.org/10.1034/j.1600-079X.2000.290303.x.
26. Ennis ZN, Dideriksen D, Vaegter HB, Handberg G, Pottegard A (2016) Acetaminophen for chronic pain: a systematic review on efficacy. Basic Clin. Pharmacol. Toxicol. 118: 184-189. DOI: 10.1111/bcpt.12527.
27. Costa D, Gomes A, Reis S, Lima JL, Fernandes E (2005) Hydrogen peroxide scavenging activity by non-steroidal anti-inflammatory drugs. Life Sci. 76: 2841-2848. DOI: 10.1016/j.lfs.2004.10.052.
28. Garner A (1992) Adaptation in the pharmaceutical industry, with particular reference to gastrointestinal damages and diseases. Scand. J. Gastroenterol. 27 (Sqpl. 193): 83 - 89.
29. Ragbetli MC, Ozyurt B, Aslan H, Odaci E, Gokcimen A, Sahin B, Kaplan S (2007) Effect of prenatal exposure to diclofenac sodium on Purkinje cell numbers in rat cerebellum: a stereological study. Brain Res. 1174: 130-135. DOI: 10.1016/j.brainres.2007.08.025.
30. Murphy PJ, Myers BL, Badia P (1996) Nonsteroidal anti-inflammatory drugs alter body temperature and suppress melatonin in humans. Physiol. Behav. 59: 133-139. https://doi.org/10.1016/0031-9384(95)02036-5.
31. Kang JH, Grodstein F (2003) Regular use of nonsteroidal anti-inflammatory drugs and cognitive function in aging women. Neurology 60: 1591-1597. DOI: https://doi.org/10.1212/01.WNL.0000065980.33594.B7.
32. Yakushiji T, Shirasaki T, Akaike N (1992) Non-competitive inhibition of GABAA responses by a new class of quinolones and non-steroidal anti-inflammatories in dissociated frog sensory neurones. Br. J. Pharmacol. 105: 13-18.
33. Vidal AC, Howard LE, Moreira DM, Castro-Santamaria R, Andriole GL, Freedland SJ (2015) Aspirin, NSAIDs, and risk of prostate cancer: results from the REDUCE study. Clin. Cancer Res. 21: 756-762. DOI: 10.1158/1078-0432.CCR-14-2235.
34. Verdoodt F, Friis S, Dehlendorff C, Albieri V, Kjaer SK (2016) Non-steroidal anti-inflammatory drug use and risk of endometrial cancer: A systematic review and meta-analysis of observational studies. Gynecol. Oncol. 140: 352-358. DOI: 10.1016/j.ygyno.2015.12.009.
35. Macfarlane TV, Lefevre K, Watson MC (2014) Aspirin and non-steroidal anti-inflammatory drug use and the risk of upper digestive tract cancer. Br. J. Cancer. 111: 1852-1859. doi: 10.1038/bjc.2014.473.
36. García Rodríguez LA, Jick H (1994) Risk of upper gastrointestinal bleeding and perforation associated with individual non-steroidal anti-inflammatory drugs. Lancet 343: 769-772. https://doi.org/10.1016/S0140-6736(94)91843-0.
37. Awtry EH, Loscalzo J (2000) Cardiovascular Drugs. Aspirin. Circulation 101: 1206-1218.
38. Bjarnason I, Scarpignato C, Takeuchi K, Rainsford KD (2007) Determinants of the short-term gastric damage caused by NSAIDs in man. Aliment. Pharmacol. Ther. 26: 95–106. DOI: 10.1111/j.1365-2036.2007.03348.x.
39. Mei Q, Diao L, Xu J, Liu X, Jin J (2011) A protective effect of melatonin on intestinal permeability is induced by diclofenac via regulation of mitochondrial function in mice. Acta Pharmacol. Sin. 32: 495–502. DOI: 10.1038/aps.2010.225.
40. Musumba C, Pritchard DM, Pirmohamed M (2011) Review article: cellular and molecular mechanisms of NSAID-induced peptic ulcers. Aliment. Pharmacol. Ther. 30: 517–531. DOI: 10.1111/j.1365-2036.2009.04086.x.
41. Tanaka A, Matsumoto M, Hayashi Y, Takeuchi K (2005) Functional mechanism underlying cyclooxygenase-2 expression in rat small intestine following administration of indomethacin: relation to intestinal hypermotility. J. Gastroenterol. Hepatol. 20: 38–45. DOI: 10.1111/j.1440-1746.2004.03520.x.
42. Tomisato W, Tsutsumi S, Hoshino T, Hwang HJ, Mio M, Tsuchiya T, Mizushima T (2004) Role of direct cytotoxic effects of NSAIDs in the induction of gastric lesions. Biochem. Pharmacol. 67: 575–85.DOI: 10.1016/j.bcp.2003.09.020.
43. Bjarnason I, Takeuchi K (2009) Intestinal permeability in the pathogenesis of NSAID-induced enteropathy. J. Gastroenterol. 44: 23–29. DOI: 10.1007/s00535-008-2266-6.
44. Kim HK, Kim JI, Kim JK, Han JY, Park SH, Choi KY, Chung IS (2007) Preventive effects of rebamipideon NSAID-induced gastric mucosal injury and reduction of gastric mucosal blood flow in healthy volunteers. Dig. Dis. Sci. 52: 1776–1782. DOI: 10.1007/s10620-006-9367-y.
45. Tanaka A, Araki H, Hase S, Komoike Y, Takeuchi K (2002) Up-regulation of COX-2 by inhibition of COX-1 in the rat: a key to NSAID-induced gastric injury. Aliment. Pharmacol. Ther. 16 (Suppl 2): 90–101.
46. Yamada T, Deitch E, Specian RB, Perry MA, Sartor RB, Grisham MB (1993) Mechanisms of acute and chronic intestinal inflammation induced by indomethacin. Inflammation 17: 641 -662.
47. Miura S, Suematsu M, Tanaka S, Nagata H, Houzawa S, Suzuki M, Kurose I, Serizawa H, Tsuchiya M (1991) Microcirculatory disturbance in indomethacin-induced intestinal ulcer. Am. J. Physioi. 261: G213 -G219. DOI: 10.1152/ajpgi.1991.261.2. G213.
48. Simmons DL, Botting RM, Hla T (2004) Cyclooxygenase isozymes: the biology of prostaglandin synthesis and inhibition. Pharmacol. Rev. 56: 387-437. DOI: 10.1124/pr.56.3.3.
49. Dey I, Lejeune M, Chadee K (2006) Prostaglandin E2 receptor distribution and function in the gastrointestinal tract. Br. J. Pharmacol. 149: 611–623. doi: 10.1038/sj.bjp.0706923.
50. Cambell, NB, Halushka PV (1996) Lipid derived autocoids. Eicosanoides and platelet activating factor. In: Hardman JG, Limbird AE, Molinoff PB, Ruddon RW, Goodman Gilman A (Eds.) Goodman & Gilman’s The Pharmacological Basis of Therapeutics. McGraw-Hill, New York, pp. 601–616.
51. Wallace JL, Cirino G (1994) The development of gastrointestinal-sparing non-steroidal anti-inflammatory drugs. Trends Pharmacol. Sci. 15: 405–406.
52. Gavalas A, Hadjipetrou L, Kourounakis P (1998) Synthesis of novel derivatives of aroyl-aminoalcohols and 3-amino-substituted 1-phenylpropanols with potential anti-inflammatory and immunomodulating activity. J. Pharm. Pharmacol. 50: 583–591. https://doi.org/10.1111/j.2042-7158.1998.tb06891.x.
53. Kukreja RC, Kontos HA, Hess ML, Ellis EF (1986) PGH synthase and lipoxygenase generate superoxide in the presence of NADH or NADPH. Circ. Res. 59: 612–619.
54. Marnett LJ (2009) The COXIB experience: a look in the rear view mirror. Annu. Rev. Pharmacol. Toxicol. 49: 265–290. DOI: 10.1146/annurev.pharmtox.011008.145638.
55. Wallace JL, McKnight W, Reuter BK, Vergnolle N (2000) NSAID-induced gastric damage in rats: requirement for inhibition of both cyclooxygenase 1 and 2. Gastroenterology 119: 706–714. https://doi.org/10.1053/gast.2000.16510.
56. Tanaka A, Araki H, Komoike Y, Hase S, Takeuchi K (2001) Inhibition of both COX-1 and COX-2 is required for development of gastric damage in response to nonsteroidal anti-inflammatory drugs. J. Physiol. Paris 95: 21–27. https://doi.org/10.1016/S0928-4257(01)00005-5.
57. Schmassmann A, Zoidl G, Peskar BM, Waser B, Schmassmann-Suhijar D, Gebbers J, Reubi JC (2006) Role of the different isoforms of cyclooxygenase and nitric oxide synthase during gastric ulcer healing in cyclooxygenase-1 and -2 knockout mice. Am. J. Physiol. Gastrointest. Liver Physiol. 290: G747–G756.
58. Mitchell JA, Akarasereenont P, Thiemermann C, Flower RJ, Vane JR (1993) Selectivity of nonsteroidal anti-inflammatory drugs as inhibitors of constitutive and inducible cyclooxygenase. Proc. Natl. Acad. Sci. U.S.A. 91: 11693-11697. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC48050.
59. Melarange R, Gentry C, Durie M, O'Connell C, and Blower PR (1994) Gastrointestinal irritancy, anti-inflammatory activity, and prostanoid inhibition in the rat: differentiation of effects between nabumetone and etdolac. Dig. Dis. Sci. 39: 601-608. https://doi.org/10.1007/BF02088349.
60. Wolfe MM, Lichenstein DR, Singh G (1999) Gastrointestinal toxicity of non-steroidal anti-inflammatory drugs. N. Engl. J. Med. 340: 1888–1899. DOI: 10.1056/NEJM199906173402407.
61. Bandyopadhyay D, Ghosh G, Bandyopadhyay A, Reiter RJ (2004) Melatonin protects against piroxicam-induced gastric ulceration. J. Pineal Res. 36: 195–203. https://doi.org/10.1111/j.1600-079X.2004.00118.x.
62. Ehrlich K, Sicking C, Respondek M, Peskar BM (2004) Interaction of cyclooxygenase isoenzymes, nitricoxide, and afferent neurons in gastric mucosal defense in rats. J. Pharmacol. Exp. Ther. 308: 277–283. DOI: 10.1124/jpet.103.057752.
63. To KF, Chan FK, Cheng AS, Lee TL, Ng YP, Sung JJ (2001) Up-regulation of cyclooxygenase-1 and-2 in human gastric ulcer. Aliment. Pharmacol. Ther. 15: 25–34. https://doi.org/10.1046/j.1365-2036.2001.00889.x.
64. Bhandari P, Bateman AC, Mehta RL, Patel P (2005) Mucosal expression of cyclooxygenase isoforms1 and 2 is increased with worsening damage to the gastric mucosa. Histopathology 46: 280–286. DOI: 10.1111/j.1365-2559.2005.02053.x.
65. Starodub OT, Demitrack ES, Baumgartner HK, Montrose MH (2008) Disruption of the Cox-1 genes lows repair of microscopic lesions in the mouse gastric epithelium. Am. J. Physiol. Cell. Physiol. 294: C223–C232. DOI: 10.1152/ajpcell.00395.2006.
66. Chan FK, Wong VW, Suen BY, et al. (2005) Effect of Celecoxib on the Healing of Complicated Gastric Ulcers: a Prospective, Double Rounded Randomised Trial (Abstract). Gasroenterology 128: A24.
67. Dikman A, Sanyal S, Von AC, Whitson M, Desai J, Bodian C, Brooks A, Bamji N, Cohen L, Miller K, Aisenberg J (2009) A randomized, placebo-controlled study of the effects of naproxen, aspirin, celecoxib or clopidogrel on gastroduodenal mucosal healing. Aliment. Pharmacol. Ther. 29: 781–91. DOI: 10.1111/j.1365-2036.2009.03928.x.
68. Wallace JL (2006) Nitricoxide, aspirin-triggered lipoxins and NO-aspirinin gastric protection. Inflamm. Allergy Drug Targets. 5: 133–137. DOI: 10.2174/187152806776383116.
69. Orrenius S (2007) Reactive oxygen species in mitochondria-mediated cell death. Drug Metab. Rev. 39: 443–55. DOI: 10.1080/03602530701468516.
70. Mashita Y, Taniguchi M, Yokota A, Tanaka A, Takeuchi K (2006) Oral but not parenteral aspirin upregulates COX-2 expression in rat stomachs: a relationship between COX-2 expression and PG deficiency. Digestion 73: 124–132. DOI: 10.1159/000094098.
71. Darling RL, Romero JJ, Dial EJ, Akunda JK, Langenbach R, Lichtenberger LM (2004) The effects of aspirin on gastric mucosal integrity, surface hydrophobicity, and prostaglandin metabolism in cyclooxygenase knockout mice. Gastroenterology 127: 94–104.https://doi.org/10.1053/j.gastro.2004.04.003.
72. Lichtenberger LM, Zhou Y, Dial EJ, Raphael RM (2006) NSAID injury to the gastrointestinal tract: evidence that NSAIDs interact with phospholipids to weaken the hydrophobic surface barrier and induce the formation of unstable pores in membranes. J. Pharm. Pharmacol. 58: 1421–1428. DOI: 10.1211/jpp.58.10.0001.
73. Barnett K, Bell CJ, McKnight W, Dicay M, Sharkey KA, Wallace JL (2000) Role of cyclooxygenase-2 in modulating gastric acid secretion in the normal and inflamed rat stomach. Am. J. Physiol. Gastrointest. Liver Physiol. 279: G1292–G1297.DOI: 10.1152/ajpgi.2000.279.6.G1292.
74. Funatsu T, Chono K, Hirata T, Keto Y, Kimoto A, Sasamata M (2007) Mucosal acid causes gastric mucosal microcirculatory disturbance in nonsteroidal anti-inflammatory drug-treated rats. Eur. J. Pharmacol. 554: 53–59. DOI: 10.1016/j.ejphar.2006.10.023.
75. Koike T, Shimada T, Fujii Y, Chen G, Tabei K, Namatame T, Yamagata M, Tajima A, Yoneda M, Terano A, Hiraishi H (2007) Upregulation of TFF1 (pS2) expression by TNF-alpha in gastric epithelial cells. J. Gastroenterol. Hepatol. 22: 936–942. DOI: 10.1111/j.1440-1746.2007.04861.x.
76. Wallace JL, Granger DN (1992) The pathogenesis of NSAIB gastropathy- are neutrophils the culprits? Trends Pharmacol. Sci. 13: 129-131.
77. Finkel T, Holbrook NJ (2000) Oxidants, oxidative stress and the biology of ageing. Nature 408: 239-247. DOI: 10.1038/35041687.
78. Yoshikawa T, Naito Y, Kishi A, Tomii T, Kaneko T, Jinuma S, Ichikawa H, Yasuda M, Takahashi S, Kondo M (1993) Role of active oxygen, lipid peroxidation, and antioxidants in the pathogenesis of gastric mucosal injury induced by indomethacin in rats. Gut 34: 732-737. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1374252.
79. Brzozowski T, Konturek PC, Konturek SJ, Pajdo R, Bielanski W, Brzozowska I, Stachura J, Han EG (1997) The role of melatonin and L-tryptophan in prevention of acute gastric lesions induced by stress, ethanol, ischemia, and aspirin. J. Pineal Res. 23: 79-89. https://doi.org/10.1111/j.1600-079X.1997.tb00339.x.
80. Das D, Bandyopadhyay D, Bhattacharjee M, Banerjee RK (1997) Hydroxyl radical is the major causative factor in stress-induced gastric ulceration. Free Radical Biol. Med. 23: 8-18.https://doi.org/10.1016/S0891-5849(96)00547-3.
81. Jou MJ, Peng TI, Hsu LF, Jou SB, Reiter RJ, Yang CM, Chiao CC, Lin YF, Chen CC (2010) Visualization of melatonin’s multiple mitochondrial levels of protection against mitochondrial Ca2+- mediated permeability transition and beyond in rat brain astrocytes. J. Pineal Res. 48: 20–38. DOI: 10.1111/j.1600-079X.2009.00721.x.
82. Motawi TK, bdElgawad HM, Shahin NN (2007) Modulation of indomethacin-induced gastric injury by spermine and taurine in rats. J. Biochem. Mol. Toxicol. 21: 280–288. DOI: 10.1002/jbt.20194.
83. Nagai N, Fukuhata T, Ito Y, Usui S, Hirano K (2009) Involvement of interleukin 18 in indomethacin-induced lesions of the gastric mucosa in adjuvant-induced arthritis rat. Toxicol. 255: 124–130.DOI: 10.1016/j.tox.2008.10.005.
84. Gallego-Sandin S, Novalbos J, Rosado A, Gisbert JP, Gálvez-Múgica MA, García AG, Pajares JM, Abad-Santos F (2004) Effect of ibuprofen on cyclooxygenase and nitric oxide synthase of gastric mucosa: correlation with endoscopic lesions and adverse reactions. Dig. Dis. Sci. 49: 1538–1544.
85. Souza SMB, Oliveira ON, Scarpa MV, Oliveira AG (2004) Study of the diclofenac/phospholipid interactions with liposomes and monolayers. Colloids Surf. B Biointerfaces 36: 13-17. DOI: 10.1016/j.colsurfb.2004.05.001.
86. Souza MH, Mota JM, Oliveira RB, Cunha FQ (2008) Gastric damage induced by different doses of indomethacin in rats is variably affected by inhibiting iNOS or leukocyte infiltration. Inflamm. Res. 57: 28–33. DOI: 10.1007/s00011-007-7089-z.
87. Mizushima T (2007) Various stress proteins protect gastric mucosal cells against non-steroidal anti-inflammatory drugs. Inflammopharmacol. 15: 67–73. DOI: 10.1007/s10787-006-1560-2.
88. Ebert MP, Schafer C, Chen J, Hoffmann J, Gu P, Kubisch C, Carl-McGrath S, Treiber G, Malfertheiner P, Röcken C (2005) Protective role of heat shock protein 27 in gastric mucosal injury. J. Pathol. 207: 177–184.DOI: 10.1002/path.1815.
89. Kusuhura H, Komatsu H, Sumichika H, Sugahara K (1999) Reactive oxygen species are involved in the apoptosis induced by nonsteroidal anti-inflammatory drugs in cultured gastric cells. Eur. J. Pharmacol. 383: 331–337.https://doi.org/10.1016/S0014-2999(99)00599-3.
90. Wilhelmsen M, Amirian I, Reiter RJ, Rosenberg J, Gögenur I (2011) Analgesic effects of melatonin: A review of current evidence from experimental and clinical studies. J. Pineal Res. 51: 270–277.DOI: 10.1111/j.1600-079X.2011.00895.x.
91. Graham DY (1990) The relationship between nonsteroidal anti-inflammatory drug use and peptic ulcer disease. Gastroenterol. Clinics. North Am. 19: 171–182.
92. May GR, Crook P, Moore PM, Page CP (1991) The role of nitric oxide as an endogenous regulator of platelet and neutrophil activation within the pulmonary circulation of the rabbit. Br. J. Pharmacol. 102: 759–763.
93. Whittle BJR (1990) Role of endogenous nitric oxide in the mechanisms underlying gastric mucosal integrity. In: Nitric oxide from L-arginine: abioregulatory system. Edited by Moncada S and Higgs EA. Elsevier Science Publishers, Amsterdam. pp. 365–371.
94. Lopez-Belmonte J, Whittle BJW, Moncada S (1993) The actions of nitric oxide donors in the prevention or induction of injury to the rat gastric mucosa. Br. J. Phamacol. 108: 73–78.
95. Reuter BK, Cirino G, Walkce JL (1994) Markedly reduced intestinal toxicity of a diclofenac derivative. Life Sci. 55: PL1-PL8.https://doi.org/10.1016/0024-3205(94)90083-3.
96. Graham DY, Agrawal NM, Roth SH (1988) Prevention of NSAID-induced gastric ulcer with misoprostol: multicentre, doubleblind, placebo-controI1d trial. Lancet 2: 1277–1288. https://doi.org/10.1016/S0140-6736(88)92892-9.
97. Soll AH, Weinstein WM, Kurata J, McCarthy D (1991) Nonsteroidal anti-inflammatory drugs and peptic ulcer disease. Ann. Intern. Med. 114: 387–319. DOI: 10.18773/austprescr.2017.037.
98. Farkouh ME, Kirshner H, Harrington RA, Ruland S, Verheugt FW, Schnitzer TJ, Burmester GR, Mysler E, Hochberg MC, Doherty M, Ehrsam E, Gitton X, Krammer G, Mellein B, Gimona A, Matchaba P, Hawkey CJ, Chesebro JH (2004) Comparison of lumiracoxib with naproxen and ibuprofen in the Therapeutic Arthritis Research and Gastrointestinal Event Trial (TARGET), cardiovascular outcomes: randomised controlled trial. Lancet 364: 675–684.DOI: 10.1016/S0140-6736(04)16894-3.
99. Maitra SK, Pal PK (2017) Melatonin rhythms in the pineal and non-pineal tissues and their physiological implications in subtropical fish. Biol. Rhythm Res. 48: 757–776.https://doi.org/10.1080/09291016.2017.1345453.
100. Pal PK, Bhattacharjee B, Ghosh A, Chattopadhyay A, Bandyopadhyay D (2018) Adrenaline induced disruption of endogenous melatonergic system, antioxidant and inflammatory responses in the gastrointestinal tissues of male Wistar rat: an in vitro study. Melatonin Research 1: 109–131. doi: 10.32794/mr11250007.
101. Raikhlin NT, Kvetnoy IM (1974) Lightening effect of the extract of human appendix mucosa on frog skin melanophores. Bull. Exp. Biol. Med. 8: 114–116.
102. Raikhlin NT, Kvetnoy IM (1976) Melatonin and enterochromaffin cells. Acta Histochem. 55: 19–25.
103. Rakhlin NT, Kvetnoy IM, Tolkachev VN (1975) Melatonin may be synthesized in enterochromafinne cells. Nature 255: 344–345.
104. Lee PPN, Shiu SYU, Chow PH, Pang SF (1995) Regional and diurnal studies on melatonin binding sites in the duck gastrointestinal tract. Biol. Signals 4: 212–224.
105. Bubenik GA (1999) Localization and physiological significance of gastrointestinal melatonin. In: R Watson (eds.) Melatonin in Health Promotion. CRC press, Boca Raton, Florida, pp. 21–39.
106. Vakkuri O, Rintamaki H, Leppaluoto J (1985a) Presence of immunoreactive melatonin in different tissues of the pigeon. Gen. Comp. Endocrinol. 58: 69–75.
107. Vakkuri O, Rintamaki H, Leppaluoto J (1985b) Plasma and tissue concentrations of melatonin after midnight light exposure and pinealectomy in the pigeon. J. Endocrinol. 105: 263–268.
108. Lee PP, Pang SF (1993) Melatonin and its receptors in the gastrointestinal tract. Biol. Signals 2: 181–193.
109. Chow PH, Lee PN, Poon AMS, Shiu SYW, Pang SF (1996) The gastrointestinal system: A site of melatonin paracrine action. In: Tang PL, Pang SF, Reiter RJ (eds.) Melatonin: A universal photoperiodic signal with diverse action. Front. Horm. Res. Basel, Karger 21: 123–132.
110. Klein D (2007) Arylalkylamine N-acetyltransferase: “the Timezyme”. J. Biol. Chem. 282: 4233–4237.DOI: 10.1074/jbc.R600036200.
111. Dobocovich M, Mankowsha M (2005) Functional MP1 and MP2 melatonin receptors in mammals. Endocrine 27: 101–110. DOI: 10.1385/ENDO:27:2:101.
112. Konturek PC, Konturek SJ, Majka J, Zembala M, Hahn EG (1997) Melatonin affords protection against gastric lesions induced by ischemia-reperfusion possibly due to its antioxidant and mucosal microcirculatory effects. Eur. J. Pharmacol. 322: 73–77. https://doi.org/10.1016/S0014-2999(97)00051-4.
113. Bubenik GA, Niles LP, Pang SF, Pentney PJ (1993) Diurnal variation and binding characteristics of melatonin in the mouse brain and gastrointestinal tissues. Comp. Biochem. Physiol. 104: 221–224. https://doi.org/10.1016/0742-8413(93)90027-I.
114. Bubenik GA, Ayles HL, Ball RO, Friendship RM, Brown GM (1998) Relationship between melatonin levels in plasma and gastrointestinal tissues and the incidence and severity of gastric ulcers in pigs. J. Pineal Res. 24:62–66. https://doi.org/10.1111/j.1600-079X.1998.tb00367.x.
115. Ercan F, Cetinel S, Contuk G, Cikler E, Sener G (2004) Role of melatonin in reducing water avoidance stress induced degeneration of the gastrointestinal mucosa. J. Pineal Res. 37: 113–121. DOI: 10.1111/j.1600-079X.2004.00143.x.
116. Srinivasan V, Lauterbach EC, Ho KY, Acuña-Castroviejo D, Zakaria R, Brzezinski A (2012) Melatonin in antinociception: Its therapeutic applications. Curr. Neuropharmacol. 10: 167–178. DOI: 10.2174/157015912800604489.
117. Becker-Andre M, Wiesenberg I, Schaeren-Wiemers N, Andre E, Missbach M, Saurat JH, Carlberg C (1994) Pineal gland hormone melatonin binds and activates an orphan of the nuclear receptor superfamily. J. Biol. Chem. 269: 28531–28534.
118. Witt-Enderby PA, Radio NM, Doctor JS, Davis VL (2006) Therapeutic treatments potentially mediated by melatonin receptors: potential clinical uses in the prevention of osteoporosis, cancer and as an adjuvant therapy. J. Pineal Res. 41: 297–305. DOI: 10.1111/j.1600-079X.2006.00369.x.
119. Boutin JA, Audinot V, Ferry G, Delagrange P (2005) Molecular tools to study melatonin pathways and actions. Trends Pharmacol. Sci. 26: 412–419. DOI: 10.1016/j.tips.2005.06.006.
120. Manchester LC, Coto-Montes A, Boga JA, Andersen LP, Zhou Z, Galano A, Vriend J, Tan DX, Reiter RJ (2015)Melatonin: an ancient molecule that makes oxygen metabolically tolerable. J. Pineal Res. 59: 403–419. DOI: 10.1111/jpi.12267.
121. Galano A, Tan DX, Reiter RJ (2018) Melatonin: a versatile protector against oxidative DNA damage.Molecules.27: 23. pii: E530. DOI: 10.3390/molecules23030530.
122. Reiter RJ, Mayo JC, Tan DX, Sainz RM, Alatorre-Jimenez M, Qin L (2016) Melatonin as an antioxidant: under promises but over delivers. J. Pineal Res. 61: 253–278. DOI: 10.1111/jpi.12360.
123. Galano A, Medina ME, Tan DX, Reiter RJ (2015) Melatonin and its metabolites as copper chelating agents and their role in inhibiting oxidative stress: a physicochemical analysis.J. Pineal Res. 58: 107–116. DOI: 10.1111/jpi.12196.
124. Reiter RJ, Rosales-Corral S, Tan DX, Jou MJ, Galano A, Xu B (2017) Melatonin as a mitochondria-targeted antioxidant: one of evolution's best ideas. Cell. Mol. Life. Sci. 74: 3863–3881. DOI: 10.1007/s00018-017-2609-7.
125. Konturek PC, Konturek SJ, Celinski K, Slomka M, Cichoz-Lach H, Bielanski W, Reiter RJ (2010) Role of melatonin in mucosal gastroprotection against aspirin-induced gastric lesions in humans .J. Pineal Res. 48: 318–323. https://doi.org/10.1111/j.1600-079X.2010.00755.x
126. Tan DX, Manchester LC, Qin L, Reiter RJ (2016) Melatonin: a mitochondrial targeting molecule involving mitochondrial protection and dynamics. Int. J. Mol. Sci.17 (12): pii: E2124. DOI: 10.3390/ijms17122124.
127. Nosál'ová V, Zeman M, Černá S, Navarová J, Zakálová M (2007) Protective effect of melatonin in acetic acid induced colitis in rats. J. Pineal Res. 42: 364–370. DOI: 10.1111/j.1600-079X.2007.00428.x
128. Torres-Farfan C, Richter HG, Rojas-García P, Vergara M, Forcelledo ML, Valladares LE, Torrealba F, Valenzuela GJ, Seron- Ferre M (2003) mt1 Melatonin receptor in the primate adrenal gland: inhibition of adrenocorticotropin-stimulated cortisol production by melatonin. J. Clin. Endocrinol. Metab. 88: 450–458. DOI: 10.1210/jc.2002-021048
129. Pal PK, Hasan NK, Maitra SK (2016) Gut melatonin response to microbial infection in carp Catlacatla. Fish Physiol. Biochem. 42: 579–592. DOI: 10.1007/s10695-015-0161-7
130. Pal PK, Maitra SK (2018) Response of gastrointestinal melatonin, antioxidants, and digestive enzymes to altered feeding conditions in carp (Catlacatla). Fish Physiol. Biochem. 44: 1061–1073. DOI: 10.1007/s10695-018-0494-0
131. Lopez-Burillo S, Tan DX, Rodriguez-Gallego V, Manchester LC, Mayo JC, Sainz RM, Reiter RJ (2003) Melatonin and its derivatives cyclic 3-hydroxymelatonin, N1-acetyl-N2-formyl-5- methoxykynuramine, and 6-hydroxymelatonin reduced oxidative damage induced by Fenton reagents. J. Pineal Res. 34: 237–256. DOI: 10.1034/j.1600-079X.2003.00025.x
132. Tomas-Zapico C, Coto-Montes A (2005) A proposed mechanism to explain the stimulatory effect of melatonin on antioxidative enzymes. J. Pineal Res. 39: 99–104. DOI: 10.1111/j.1600-079X.2005.00248.x
133. El-Sokkary GH, Kamel ES, Reiter RJ (2003) Prophylactic effect of melatonin in reducing lead-induced neurotoxicity in the rat. Cell. Mol. Biol. Lett. 8: 461-470.
134. León J, Acuña-Castroviejo D, Escames G, Tan DX, Reiter RJ (2005) Melatonin mitigates mitochondrial malfunction. J. Pineal Res. 38: 1–9. DOI: 10.1111/j.1600-079X.2004.00181.x
135. Martín M, Macías M, León J, Escames G, Khaldy H, Acuña- Castroviejo D (2002) Melatonin increases the activity of the oxidative phosphorylation enzymes and the production of ATP in rat brain and liver mitochondria. Int. J. Biochem. Cell. Biol. 34: 348–357.
136. Acuña-Castroviejo D, Escames G, León J, Carazo A, Khaldy H (2003) Mitochondrial regulation by melatonin and its metabolites. Adv. Exp. Med. Biol. 527: 549–557.
137. Hussein MR, Abu-Dief EE, Abd El-Reheem MH, Abd-Elrahman A (2005) Ultrastructural evaluation of the radioprotective effects of melatonin against X-ray-induced skin damage in Albino rats. Int. J. Exp. Pathol. 86: 45–55. DOI: 10.1111/j.0959-9673.2005.00412.x
138. Sener G, Sert G, Sehirli AO, Arbak S, Gedik N, Ayanoglu-Dülger G (2006) Melatonin protects against pressure ulcer-induced oxidative injury of the skin and remote organs in rats. J. Pineal Res. 40: 280–287. DOI: 10.1111/j.1600-079X.2005.00313.x
139. Maity P, Bindu S, Dey S, Goyal M, Alam A, Pal C, Reiter R, Bandyopadhyay U (2009) Melatonin reduces indomethacin-induced gastric mucosal cell apoptosis by preventing mitochondrial oxidative stress and the activation of mitochondrial pathway of apoptosis. J. Pineal Res. 46: 314–323.
140. Konturek PC, Konturek SJ, Ketal C (2004) Role of melatonin in mucosal gastroprotection against aspirin-induced gastric lesions in human. J. Pineal Res. 48: 318–323.
141. Cabeza J, Alarcón-de-la-Lastra C, Jiménez D, Martín MJ, Motilva V (2003) Melatonin modulates the effects of gastric injury in rats: role of prostaglandins and nitric oxide. Neurosignals 12: 71–77.
142. Ozturk H, Oztürk H, Yagmur Y, Uzunlar AK (2006) Effects of melatonin administration on intestinal adaptive response after massive bowel resection in rats. Dig. Dis. Sci. 51: 333–337. DOI: 10.1007/s10620-006-3134-y
143. Voisin P, Van Camp G, Pontoire C, Collin JP (1993) Prostaglandins stimulate serotonin acetylation in chick pineal ceils: involvement of cyclic AMP-dependent and calcium/calmodulin-dependent mechanisms. J. Neurochem. 60: 666–670.
144. Pandi-Perumal SR, Srinivasan V, Maestroni GJ, Cardinali DP, Poeggeler B, Hardeland R (2006) Melatonin: Nature's most versatile biological signal? FEBS J. 273: 2813–2838. DOI: 10.1111/j.1742-4658.2006.05322.x
145. Konturek PC, Konturek SJ, Burnat G, Brzozowski T, Brzozowska I, Reiter RJ (2008) Dynamic physiological and molecular changes in gastric ulcer healing achieved by melatonin and its precursor L-tryptophan in rats. J. Pineal Res. 45: 180–190. DOI: 10.1111/j.1600-079X.2008.00574.x
146. Brzozowska I, Konturek PC, Brzozowski T, KonturekSJ, Kwiecien S, Pajdo R, Drozdowicz D, Pawlik M, Ptak A, Hahn EG (2002) Role of prostaglandins, nitric oxide, sensory nerves and gastrin in acceleration of ulcer healing by melatonin and its precursor, L-tryptophan. J. Pineal Res. 32: 149–162.
147. Hardeland R, Tan DX, Reiter RJ (2009) Kynuramines, metabolites of melatonin and other indoles:the resurrection of an almost forgotton class of biogenic amines. J. Pineal Res. 47: 109–124. DOI: 10.1111/j.1600-079X.2009.00701.x
148. Gitto E, Pellegrino S, Gitto P, Barberi I, Reiter RJ (2009) Oxidative stress of the newborn in the pre-and postnatal period and the clinical utility of melatonin. J. Pineal Res. 44: 128–139. DOI: 10.1111/j.1600-079X.2008.00649.x
149. Odaci E and Kaplan S (2009) Melatonin and nerve regeneration. Int. Rev. Neurobiol. 87: 317–335. DOI: 10.1016/S0074-7742(09)87016-5
150. Chen LJ, Gao YQ, Li XJ, Shen DH, Sun FY (2005) Melatonin protects against MPTP/MPP+ -induced mitochondrial DNA oxidative damage in vivo and in vitro. J. Pineal Res. 39: 34–42. DOI: 10.1111/j.1600-079X.2005.00209.x
151. Jaworek J, Brzozowski T, Konturek SJ (2005) Melatonin as an organoprotector in the stomach and the pancreas. J. Pineal Res. 38: 73–83. DOI: 10.1111/j.1600-079X.2004.00179.x
152. Ganguly K, Maity P, Reiter RJ, Swarnakar S (2005) Effect of melatonin on secreted and induced matrix metalloproteinase -9 and -2 activity during prevention of indomethacin-induced gastric ulcer. J. Pineal Res. 39: 307–315. DOI: 10.1111/j.1600-079X.2005.00250.x
153. Ganguly K, Kundu P, Banerjee A, Reiter RJ, Swarnakar S (2006) Hydrogenperoxide-mediated down regulation of matrixmetalloprotease-2 in indomethacin-induced acute gastric ulceration is blocked by melatonin and other antioxidants. Free Radic. Biol. Med. 41: 911–925. https://doi.org/10.1016/j.freeradbiomed.2006.04.022
154. Brzozowska I, Konturek PC, Brzozowski T, Konturek SJ, Kwiecien S, Pajdo R, Drozdowicz D, Pawlik M, Ptak A, Hahn EG (2002) Role of prostaglandins, nitric oxide, sensory nerves and gastrin in acceleration of ulcer healing by melatonin and its precursor, L-tryptophan. J. Pineal Res. 32: 149–162. https://doi.org/10.1034/j.1600-079x.2002.1o811.x
155. Brzozowski T, Konturek PC, ZwirskaKorczala K, Konturek SJ, Brzozowska I, Drozdowicz D, Sliwowski Z, Pawlik M, Pawlik WW, Hahn EG (2005) Importance of the pineal gland, endogenous prostaglandins and sensory nerves in the gastroprotective actions of central and peripheral melatonin against stress-induced damage. J. Pineal Res. 39: 375–385. https://doi.org/10.1111/j.1600-079X.2005.00264.x
156. Sjoblom M, Flemstrom G (2003) Melatonin in the duodenal lumen is a potent stimulant of mucosal bicarbonate secretion. J. Pineal Res. 34: 288–293. https://doi.org/10.1034/j.1600-079X.2003.00044.x
157. Hernández-Pacheco A, Araiza-Saldaña CI, Granados-Soto V and Mixcoatl-Zecuatl T (2008) Possible participation of the nitric oxide-cyclic GMP-protein kinase G-K+ channels pathway in the peripheral antinociception of melatonin. Eur. J. Pharmacol. 596: 70–76. DOI: 10.1016/j.ejphar.2008.07.068.
158. Marseglia L, D'Angelo G, Manti S, Aversa S, Arrigo T, Reiter RJ, Gitto E (2015) Analgesic, anxiolytic and anaesthetic effects of melatonin: New potential uses in pediatrics. Int. J. Mol. Sci. 16: 1209–1220. DOI: 10.3390/ijms16011209.
159. Rocha N, Rotelli A, Aguilar CF, Pelzer L (2007) Structural Basis of the Anti-inflammatory. Arzneimittel-Forschung/Drug Research 57: 782–786. DOI: 10.1055/s-0031-1296680.
160. Maity P, Bindu S, Dey S, Goyal M, Alam A, Pal C, Reiter RJ, Bandyopadhyay U (2009) Melatonin reduces indomethacin‐induced gastric mucosal cell apoptosis by preventing mitochondrial oxidative stress and the activation of mitochondrial pathway of apoptosis. J. Pineal Res. 46: 314–323. DOI: 10.1111/j.1600-079X.2009.00663.x.

This work is licensed under a Creative Commons Attribution 4.0 International License.
For all articles published in Melatonin Res., copyright is retained by the authors. Articles are licensed under an open access Creative Commons CC BY 4.0 license, meaning that anyone may download and read the paper for free. In addition, the article may be reused and quoted provided that the original published version is cited. These conditions allow for maximum use and exposure of the work, while ensuring that the authors receive proper credit.
In exceptional circumstances articles may be licensed differently. If you have specific condition (such as one linked to funding) that does not allow this license, please mention this to the editorial office of the journal at submission. Exceptions will be granted at the discretion of the publisher.


