Daytime orexin and night-time melatonin regulation of mitochondria melatonin: roles in circadian oscillations systemically and centrally in breast cancer symptomatology
Melatonin and breast cancer
Abstract
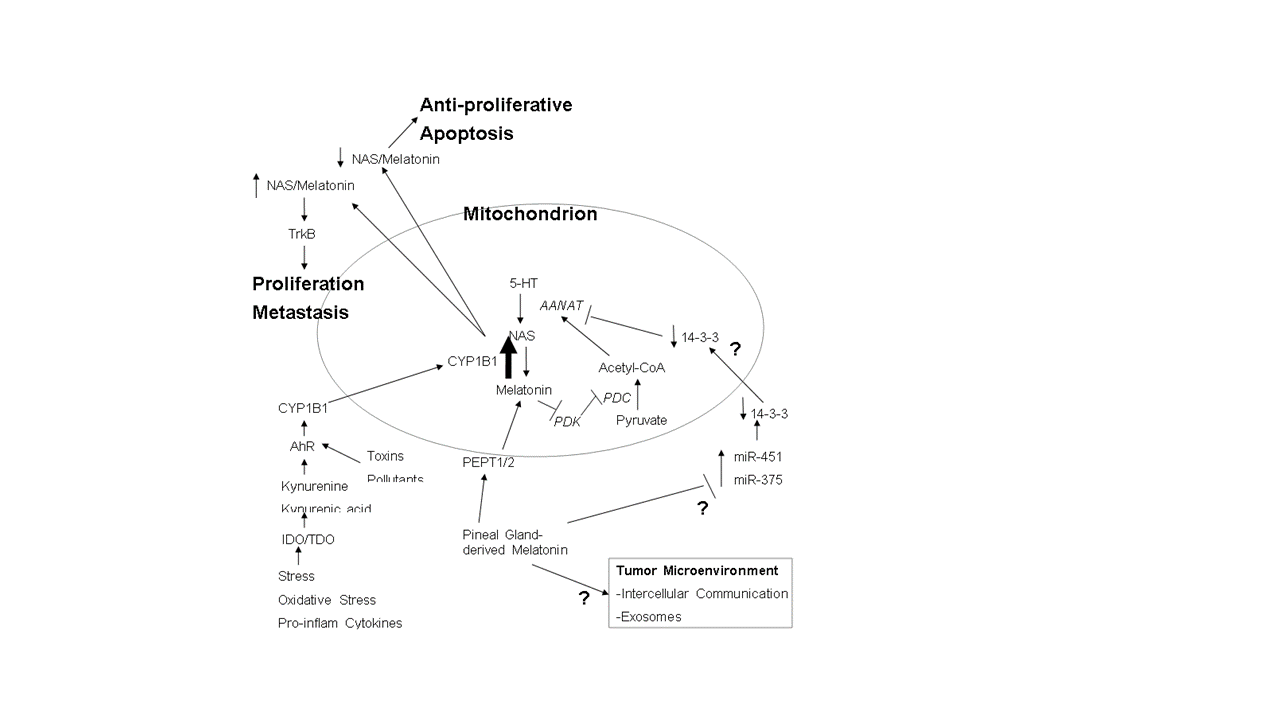
This article reviews the recent proposed model of Reiter and colleagues in this journal on the role of circadian, pineal gland-derived melatonin in driving mitochondria melatonin production in the pathoetiology and pathophysiology of breast cancers. This uptake of melatonin is proposed to inhibit pyruvate dehydrogenase kinase, thereby increasing the production of acetyl-CoA from pyruvate, with acetyl-CoA being a necessary co-factor for the initiation of the melatonergic pathway within mitochondria. Consequently, this proposed model suggests that a circadian shift in metabolic regulation occurs in breast cancers, from daytime cytosolic glycolysis to a night-time, melatonin-driven mitochondria oxidative phosphorylation, with relevance to the early pathoetiology of breast cancers. This has a number of consequences and links well to wider breast cancer data showing a pathophysiological role for the aryl hydrocarbon receptor, cytochrome P450 (CYP)1B1, 14-3-3 protein, and microRNAs. The current article overviews such data in the context of pineal gland-derived melatonin's circadian regulation of the mitochondria melatonergic pathways in breast cancer cells as proposed by Reiter and colleagues, suggesting that daytime, wake promoting orexin and stress-induced gut dysregulation contribute to mitochondria dysfunction in wider breast cancer symptomatology.
References
2. Reiter RJ, Sharma R, Ma Q, Rosales-Corral SA, Acuna-Castroviejo D, Escames G (2019) Inhibition of mitochondrial pyruvate dehydrogenase kinase: a proposed mechanism by which melatonin causes cancer cells to overcome aerobic glycolysis, limit tumor growth and reverse insensitivity to chemotherapy. Melatonin Res. 2 (3): 105-119. doi:10.32794/mr11250033.
3. Suofu Y, Li W, Jean-Alphonse FG et al. (2017) Dual role of mitochondria in producing melatonin and driving GPCR signaling to block cytochrome c release. Proc. Natl. Acad. Sci. USA 114: E7997-E8006.
4. Lellupitiyage Don SS, Lin HH, Furtado JJ, et al. (2019) Circadian oscillations persist in low malignancy breast cancer cells. Cell Cycle. 18 (19): 2447-2453. doi:10.1080/15384101.2019.1648957.
5. Neufeld-Cohen A, Robles MS, Aviram R, et al. (2016) Circadian control of oscillations in mitochondrial rate-limiting enzymes and nutrient utilization by PERIOD proteins. Proc. Natl. Acad. Sci. U S A. 113 (12): E1673-82. doi:10.1073/pnas.1519650113.
6. Groza M, Zimta AA, Irimie A, et al. (In press) Recent advancements in the study of breast cancer exosomes as mediators of intratumoral communication. J. Cell Physiol. doi: 10.1002/jcp.29096.
7. Yu X, Zhang Q, Zhang X, et al. (2019) Exosomes from Macrophages Exposed to Apoptotic Breast Cancer Cells Promote Breast Cancer Proliferation and Metastasis. J. Cancer 10 (13): 2892-2906. doi:10.7150/jca.31241.
8. Cheng L, Liu J, Liu Q, et al. (2017) Exosomes from melatonin treated hepatocellular carcinoma cells alter the immunosupression status through STAT3 pathway in macrophages. Int. J. Biol. Sci. 13 (6): 723-734. doi:10.7150/ijbs.19642.
9. Coelho LA, Andrade-Silva J, Motta-Teixeira LC, Amaral FG, Reiter RJ, Cipolla-Neto J. (In press) The absence of pineal melatonin abolishes the daily rhythm of tph1 (tryptophan hydroxylase 1), ASMT (acetylserotonin o-methyltransferase), and AANAT (aralkylamine n- acetyltransferase) mRNA expressions in rat testes. Mol. Neurobiol. doi: 10.1007/s12035- 019-1626-y.
10. Muxel SM, Pires-Lapa MA, Monteiro AW, et al. (2012) NF-κB drives the synthesis of melatonin in RAW 264.7 macrophages by inducing the transcription of the arylalkylamine-N-acetyltransferase (AA-NAT) gene. PLoS One. 7 (12): e52010. doi: 10.1371/journal.pone.0052010.
11. Jang SW, Liu X, Pradoldej S, et al. (2010) N-acetylserotonin activates TrkB receptor in a circadian rhythm. Proc. Natl. Acad. Sci. U S A. 107 (8): 3876-81. doi: 10.1073/pnas.0912531107.
12. Anderson G (2019) Breast cancer: Occluded role of mitochondria N-acetylserotonin/melatonin ratio in co-ordinating pathophysiology. Biochem. Pharmacol. 168: 259-268. doi:10.1016/j.bcp.2019.07.014.
13. Anderson G, Reiter RJ. (2019) Glioblastoma: role of mitochondria n-acetylserotonin/melatonin ratio in mediating effects of mir-451 and aryl hydrocarbon receptor and in coordinating wider biochemical changes. Int. J. Tryptophan Res. 12: 1178646919855942. doi:10.1177/1178646919855942.
14. Qu X, Metz RP, Porter WW, Cassone VM, Earnest DJ. (2007) Disruption of clock gene expression alters responses of the aryl hydrocarbon receptor signaling pathway in the mouse mammary gland. Mol. Pharmacol. 72 (5): 1349-1358.
15. Pagan C, Goubran-Botros H, Delorme R, et al. (2017) Disruption of melatonin synthesis is associated with impaired 14-3-3 and miR-451 levels in patients with autism spectrum disorders. Sci. Rep. 7 (1): 2096. doi:10.1038/s41598-017-02152-x.
16. Wang W, Zhang L, Wang Y, et al. (2017) Involvement of miR-451 in resistance to paclitaxel by regulating YWHAZ in breast cancer. Cell Death Dis. 8 (10): e3071. doi: 10.1038/cddis.2017.460.
17. Liu Y, Zhao Y, Guo L. (2016) Effects of orexin A on glucose metabolism in human hepatocellular carcinoma in vitro via PI3K/Akt/mTOR-dependent and -independent mechanism. Mol Cell Endocrinol. 420: 208-16. doi:10.1016/j.mce.2015.11.002.
18. Sharma R, Sahota P, Thakkar MM. (2018) Melatonin promotes sleep in mice by inhibiting orexin neurons in the perifornical lateral hypothalamus. J. Pineal Res. 65 (2): e12498. doi:10.1111/jpi.12498.
19. Mikkelsen JD, Hauser F, deLecea L, et al. (2001) Hypocretin (orexin) in the rat pineal gland: a central transmitter with effects on noradrenaline-induced release of melatonin. Eur. J. Neurosci. 14 (3): 419-425.
20. Borniger JC, Walker Ii WH, et al. (2018) A role for hypocretin/orexin in metabolic and sleep abnormalities in a mouse model of non-metastatic breast cancer. Cell Metab. 28 (1): 118-129.e5. doi:10.1016/j.cmet.2018.04.021.
21. Li P, Huang J, Wu H, et al. (2016) Impact of lifestyle and psychological stress on the development of early onset breast cancer. Medicine (Baltimore). 95 (50): e5529.
22. Pontes GN, Cardoso EC, Carneiro-Sampaio MM, Markus RP. (2007) Pineal melatonin and the innate immune response: the TNF-alpha increase after caesarean section suppresses nocturnal melatonin production. J. Pineal Res. 43 (4): 365-371.
23. Anderson G. (2019) Gut dysbiosis dysregulates central and systemic homeostasis via decreased melatonin and suboptimal mitochondria functioning: pathoetiological and pathophysiological implications. Melatonin Res. 2 (2): 70-85; doi:10.32794/mr11250022
24. Fetisova EK, Muntyan MS, Lyamzaev KG, Chernyak BV. (2019) Therapeutic effect of the mitochondria-targeted antioxidant skq1 on the culture model of multiple sclerosis. Oxid. Med. Cell Longev. 2019: 2082561. doi:10.1155/2019/2082561.
25. Castillo SS, Levy M, Thaikoottathil JV, Goldkorn T. (2007) Reactive nitrogen and oxygen species activate different sphingomyelinases to induce apoptosis in airway epithelial cells. Exp. Cell Res. 313 (12): 2680-2686.
26. Rambold AS, Pearce EL. (2018) Mitochondrial dynamics at the interface of immune cell metabolism and function. Trends Immunol. 39 (1): 6-18. doi:10.1016/j.it.2017.08.006.
27. Moro K, Nagahashi M, Gabriel E, Takabe K, Wakai T. (2019) Clinical application of ceramide in cancer treatment. Breast Cancer 26 (4): 407-415. doi:10.1007/s12282-019-00953-8.
28. Pozuelo-Rubio M. (2010) Proteomic and biochemical analysis of 14-3-3-binding proteins during C2-ceramide-induced apoptosis. FEBS J. 277 (16): 3321-3342. doi: 10.1111/j.1742-4658.2010.07730.x.

This work is licensed under a Creative Commons Attribution 4.0 International License.
For all articles published in Melatonin Res., copyright is retained by the authors. Articles are licensed under an open access Creative Commons CC BY 4.0 license, meaning that anyone may download and read the paper for free. In addition, the article may be reused and quoted provided that the original published version is cited. These conditions allow for maximum use and exposure of the work, while ensuring that the authors receive proper credit.
In exceptional circumstances articles may be licensed differently. If you have specific condition (such as one linked to funding) that does not allow this license, please mention this to the editorial office of the journal at submission. Exceptions will be granted at the discretion of the publisher.


